The AJCC staging system for conjunctival carcinoma remains largely unchanged from the AJCC Cancer Staging Manual, 7th Edition, apart from a more precisely defined disease extent for early invasive lesions (T1 and T2). This change has implications for management, as emerging studies support adjuvant treatment in some of these patients.
It is acknowledged that the TNM staging system for these tumors would benefit greatly from the establishment of multicenter registries, prospective rand omized trials, and prospective data mining to consolidate and expand the definitions of prognostic significance and to incorporate biomarkers.
Similarly, it is noted that data from a large registry would help provide significance to the currently applied subdivisions of intraepithelial disease (i.e., conjunctival squamous intraepithelial neoplasia, I-III). However, these data currently do not exist.
AJCC staging for conjunctival carcinoma is becoming more important, because the incidence of conjunctival squamous cell carcinoma (SCC) associated with HIV is increasing, especially in younger individuals in developing countries with high incidences of HIV. Such tumors behave more aggressively.
This chapter clearly defines the clinical term ocular squamous surface neoplasia and explains why a histopathologic tissue diagnosis is needed for TNM staging.
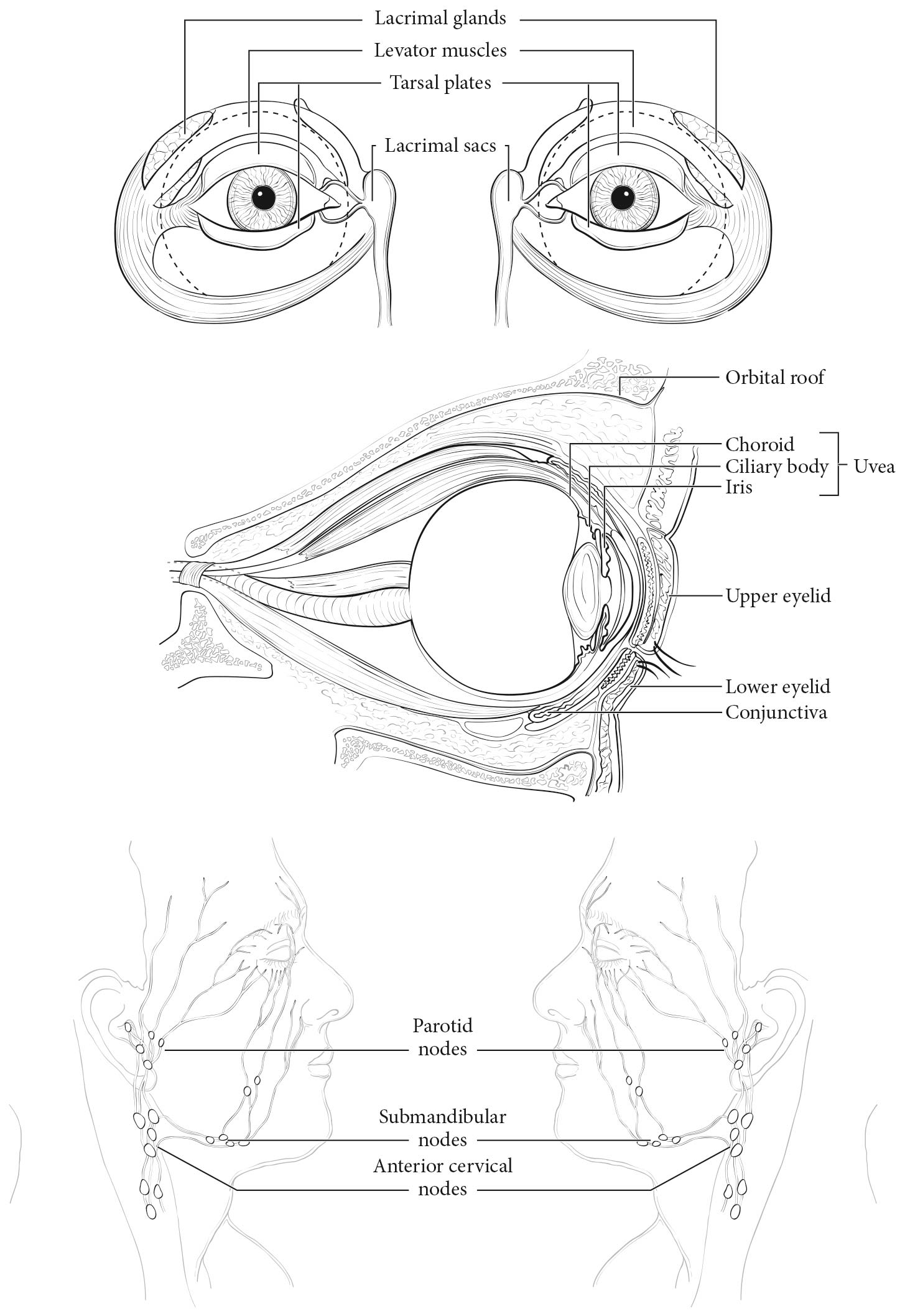
This staging system applies to conjunctival carcinoma comprising predominantly SCC and corneal squamous intraepithelial neoplasia, along with other histologic subtypes (see ICD-O-3 Histology Codes). Nonepithelial tumors of the conjunctiva are not staged using these criteria. Biopsy is required for tumor staging.
Risk factors for the disease are exposure to sun and ultraviolet B light, as well as light-colored skin. Other risk factors include radiation exposure, smoking, human papillomavirus (HPV) infection, chemical exposures, immunosuppression, and particular syndromes (e.g., xeroderma pigmentosum). In developed countries, this condition is more common in men, with a peak incidence in the seventh decade of life. At diagnosis, it is typically localized to the corneal limbus. Conjunctival carcinoma also is associated with HIV infection, and this association is particularly prevalent in developing countries, where it may be considered an AIDS-defining illness, especially in younger patients.1-10
Ocular surface squamous neoplasia is a clinical term encompassing the continuum of disease from mild epithelial dysplasia to SCC. Because this term includes overlapping histopathologic grades and entities, it is imprecise and should be avoided in histopathology reports. The precise morphologic changes should be documented using terminology applied in pathology. 11,12
After clinical and pathological diagnosis, excisional treatment typically is supplemented by adjunctive double freeze-thaw cryotherapy to the conjunctival margins and sclera base at the time of primary resection.13 Additional adjuvant and /or alternative treatments include topical chemotherapy (mitomycin C, 5-fluorouracil, or interferon alfa-2b). Radiation therapy (teletherapy or brachytherapy) may be used when complete resection is not possible or as salvage treatment to avoid orbital exenteration.14-20