- Determine rhythm.
- Atrial rhythm:
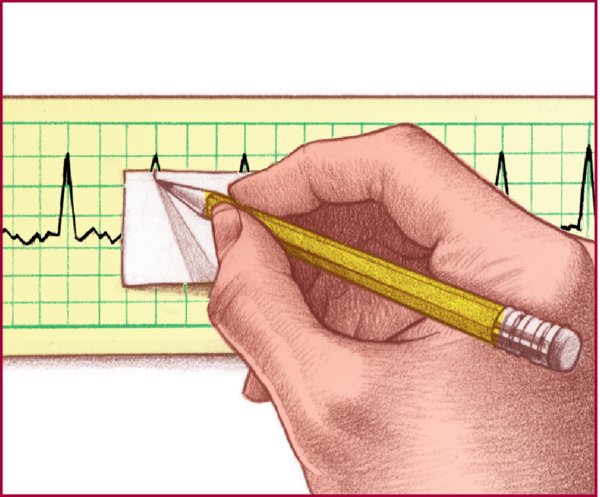
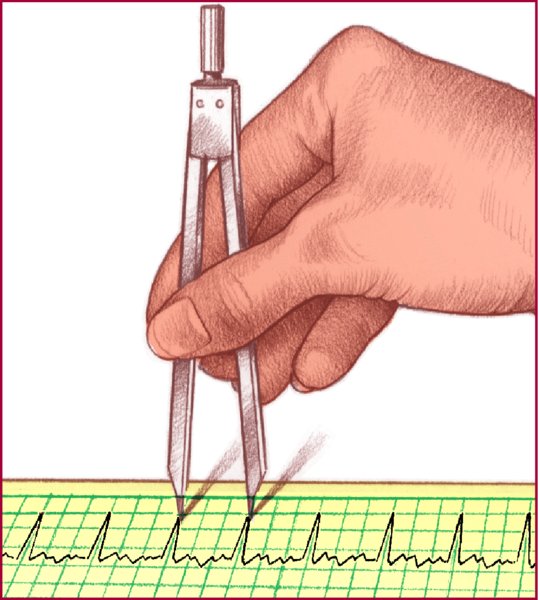
- Measure P-P intervals for several cycles.
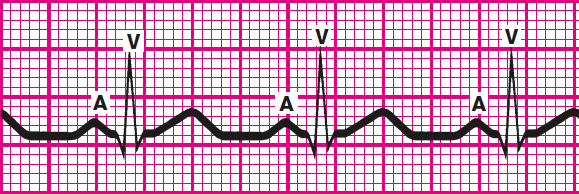
- If consistently similar, atrial rhythm is regular.
- If dissimilar, atrial rhythm is irregular.
- Measure P-P intervals for several cycles.
- Ventricular rhythm:
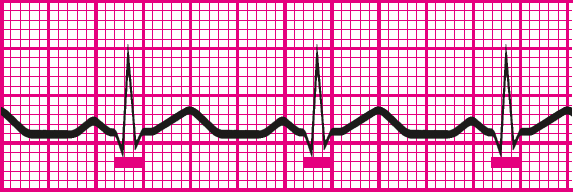
- Measure the intervals between two consecutive R waves in the QRS complexes.
- If no R wave, use the Q wave or the S wave of consecutive QRS complexes.
- If R-R intervals are consistently similar, ventricular rhythm is regular.
- If dissimilar, ventricular rhythm is irregular.
- Atrial rhythm:
- Calculate rate using one of three methods: times-10; 1,500; or sequence.
- Times-10 method
- Obtain a 6-second strip.
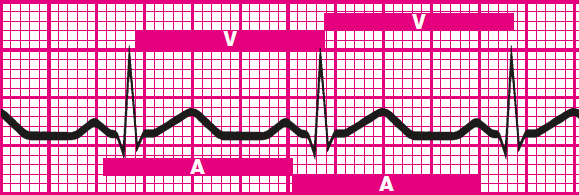
- Count the number of P waves.
- Multiply the number of P waves by 10 (ten, 6-second strips equal 1 minute) to calculate the atrial rate.
- Calculate ventricular rate the same way using R waves.
- Obtain a 6-second strip.
- 1,500 method (because 1,500 small squares equal 1 minute)
- Count the number of small squares between identical points on two consecutive P waves.
- Divide the number by 1,500 to get the atrial rate.
- Use the same method with two consecutive R waves to calculate the ventricular rate.
- Sequence method
- Find a P wave that peaks on a heavy black line.
- Assign these numbers to the next six heavy black lines: 300, 150, 100, 75, 60, and 50.
- Find the next P wave peak.
- Estimate the atrial rate based on the number assigned to the nearest heavy black line.
- Estimate the ventricular rate the same way using the R wave.
- Times-10 method
- Evaluate P wave.
- Determine if a P wave is present for every QRS complex.
- Assess whether it has a normal configuration, size, and shape.
- Determine if a P wave is present for every QRS complex.
- Determine PR interval duration.
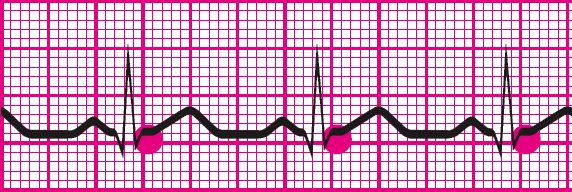
- Count the small squares between the start of the P wave and the start of the QRS complex.
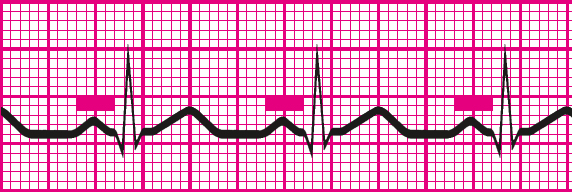
- Multiply the number of squares by 0.04 second.
- Determine if the duration is normal (0.12 to 0.20 second, or 3 to 5 small squares) and consistent.
- Count the small squares between the start of the P wave and the start of the QRS complex.
- Determine QRS complex duration.
- Measure straight across from the beginning of the QRS complex to the end of the S wave (not just to the peak).
- Count the small squares between the beginning and end of the QRS complex.
- Multiply this number by 0.04 second.
- Determine if the duration is normal (0.06 to 0.12 second); all QRS complexes are the same size and shape, and a complex appears after every P wave.
- Measure straight across from the beginning of the QRS complex to the end of the S wave (not just to the peak).
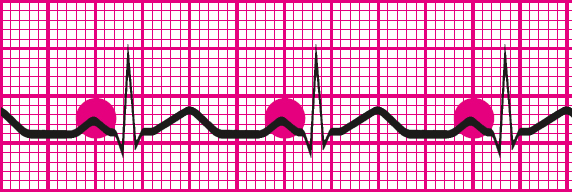
- Evaluate T wave.
- Determine if T waves are present and have a normal shape, normal amplitude, and the same deflection as the QRS complexes.
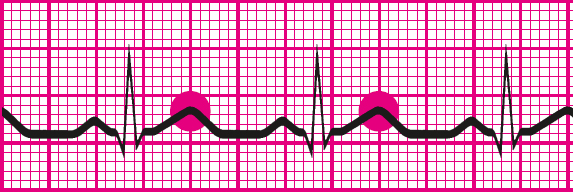
- Consider whether a P wave could be hidden in a T wave.
- Determine if T waves are present and have a normal shape, normal amplitude, and the same deflection as the QRS complexes.
- Determine QT interval duration.
- Count the small squares between the beginning of the QRS complex and the end of the T wave (where the T wave returns to the baseline).
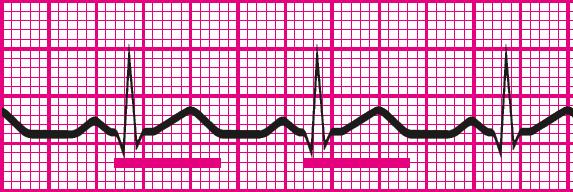
- Multiply this number by 0.04 second.
- Determine if the duration is normal (0.36 to 0.44 second).
- Count the small squares between the beginning of the QRS complex and the end of the T wave (where the T wave returns to the baseline).
- Evaluate other components.
- Make sure that the waveform doesn't reflect problems with the monitor (see pages 28 to 31).
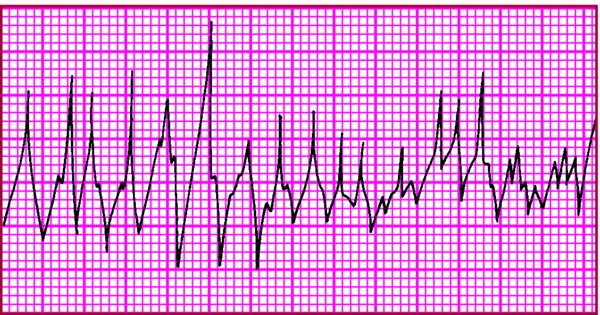
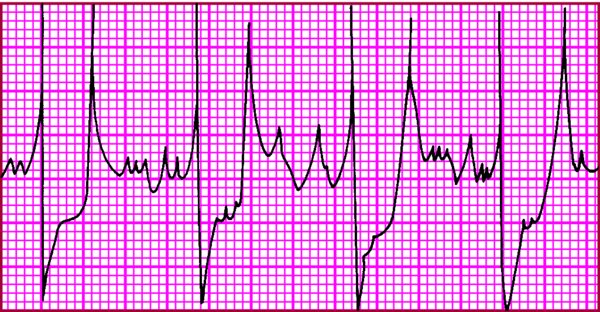
- Note ectopic beats, aberrantly conducted beats, or other abnormalities.
- Check the ST segment for abnormalities.
- Look for a U wave.
- Classify the rhythm strip according to one or all of the following characteristics:
- Site of origin of the rhythm (sinus node, atria, AV node, or ventricles)
- Rate (normal [60 to 100 beats/min], bradycardic [less than 60 beats/min], tachycardic [more than 100 beats/min])
- Rhythm (regular or irregular [flutter, fibrillation, heart block, escape rhythm, other arrhythmias]).
- Make sure that the waveform doesn't reflect problems with the monitor (see pages 28 to 31).
|

Correcting the QT interval The QT interval is affected by the patient's heart rate. As the heart rate increases, the QT interval decreases; as the heart rate decreases, the QT interval increases. For this reason, evaluating the QT interval based on a standard heart rate of 60 is recommended. This corrected QT interval is known as QTc. The following formula is used to determine the QTc: 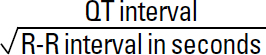 The normal QTc for women is less than 0.45 second and for men is less than 0.43 second. When the QTc is longer than 0.50 second in men or women, torsades de pointes is more likely to develop. |
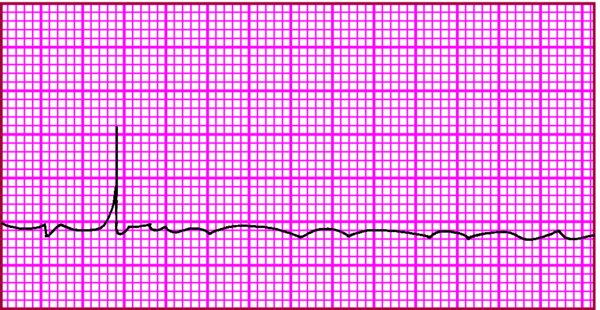
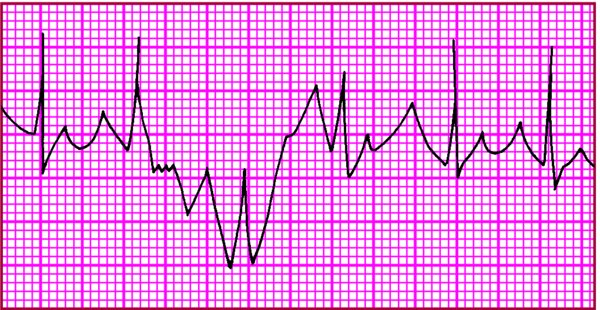
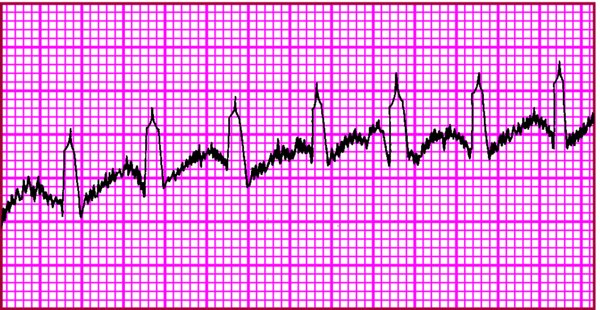
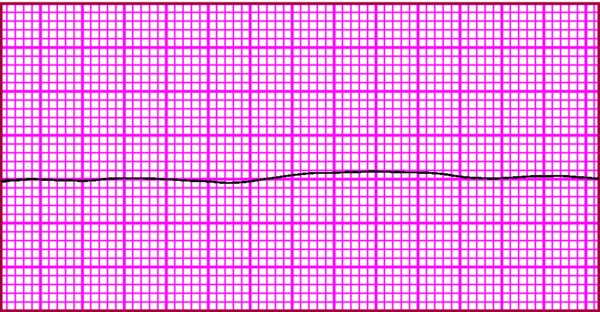
Identifying monitor problems Abnormal waveforms could indicate monitor problems. This chart reviews commonly encountered problems, their possible causes, and suggested interventions. Remember, however, you should always assess the patient before troubleshooting the equipment.
|