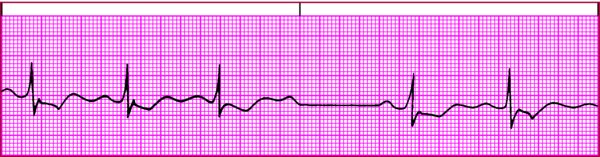
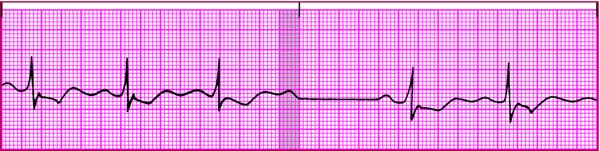
Distinguishing type II second-degree AV block from nonconducted PACs An isolated nonconducted P wave (a P wave not followed by a QRS complex, as shown in the shaded areas below) may result from type II second-degree AV block or a nonconducted PAC. Confusing these two arrhythmias can have serious consequences. The former is usually benign, but the latter can be life-threatening. Second-degree AV block type II 
If the P-P interval is constant, including the extra P wave, it's type II second-degree AV block. Nonconducted PAC 
If the P-P interval, including the extra P wave, isn't constant, it's a nonconducted PAC. |