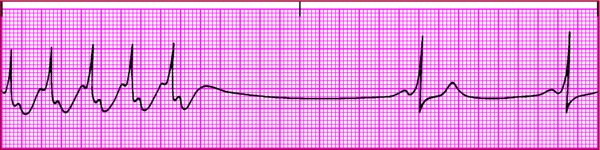
- Cardiomyopathy
- Heart block
- Inferior-wall MI
- Myocardial ischemia
- Myocarditis
- Sinoatrial (SA) node disease
- Conditions that increase vagal stimulation or decrease sympathetic stimulation
- Carotid sinus massage
- Deep relaxation
- Sleep
- Valsalva maneuver
- Vomiting
- Glaucoma
- Hyperkalemia
- Hypothermia
- Hypothyroidism
- Increased ICP
- Drugs
- Antiarrhythmics (amiodarone [Cordarone], propafenone [Rythmol], quinidine, sotalol [Betapace])
- Beta-adrenergic blockers (metoprolol [Lopressor], propranolol [Inderal])
- Calcium channel blockers (diltiazem [Diltiazem], verapamil [Calan])
- Digoxin (Lanoxin)
- Lithium (Lithobid)
- Normal in well-conditioned athletes