Recognizing sinus arrest 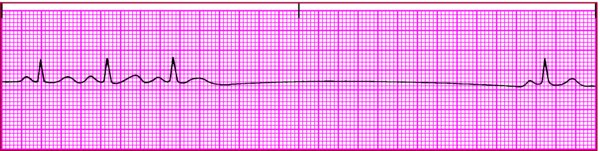
Rhythm - Regular except during arrest (irregular as result of missing complexes)
Rate - Usually within normal limits (60 to 100 beats/min) before arrest
- Length or frequency of pause may result in bradycardia
P wave - Periodically absent, with entire PQRST complexes missing
- When present, normal size and configuration
- Precedes each QRS complex
PR interval - Within normal limits when a P wave is present
- Constant when a P wave is present
QRS complex - Normal duration
- Normal configuration
- Absent during arrest
T wave - Normal size
- Normal configuration
- Absent during arrest
QT interval - Within normal limits
- Absent during arrest
Other - The pause isn't a multiple of the underlying P-P intervals
- Junctional escape beats may occur at end of pause
|
