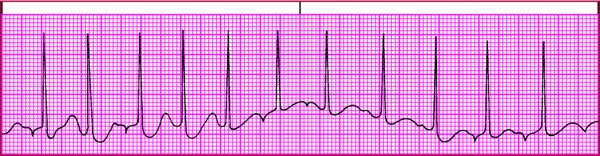
Identifying types of atrial tachycardia Atrial tachycardia comes in three varieties. Here's a quick rundown of each. Atrial tachycardia with block Atrial tachycardia with block is caused by increased automaticity of the atrial tissue. As the atrial rate speeds up and AV conduction becomes impaired, a 2:1 block typically occurs. Occasionally a type I (Wenckebach) second-degree AV block may be seen. Look for these distinguishing characteristics: 
Rhythm - Atrial—regular; ventricular—regular if block is constant, irregular if block is variable
Rate - Atrial—150 to 250 beats/min, multiple of ventricular rate; ventricular—varies with block
P wave - Slightly abnormal; shape depends on site of ectopic pacemaker
PR interval T wave - Usually indistinguishable
Other - More than one P wave for each QRS complex
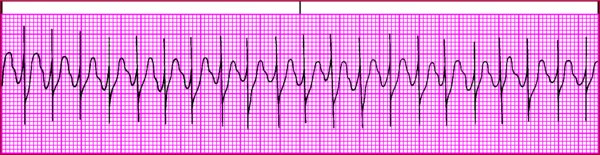
Multifocal atrial tachycardia In MAT, atrial tachycardia occurs with numerous atrial foci firing intermittently. MAT produces varying P waves on the strip and occurs most commonly in patients with chronic pulmonary disease. The irregular baseline in this strip is caused by movement of the chest wall. Look for these distinguishing characteristics: 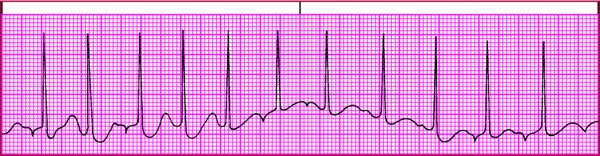
Rhythm - Atrial and ventricular—irregular
Rate - Atrial—100 to 250 beats/min, usually under 160; ventricular—100 to 250 beats/min
P wave - Configuration varies; must see at least three different P wave shapes
QRS complex - Usually normal; can be aberrant if arrhythmia persists
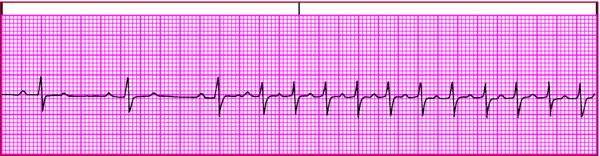
Paroxysmal atrial tachycardia A type of paroxysmal supraventricular tachycardia, PAT features brief periods of tachycardia that alternate with periods of normal sinus rhythm. PAT starts and stops suddenly as a result of rapid firing of an ectopic focus. It commonly follows frequent PACs, one of which initiates the tachycardia. Look for these distinguishing characteristics: 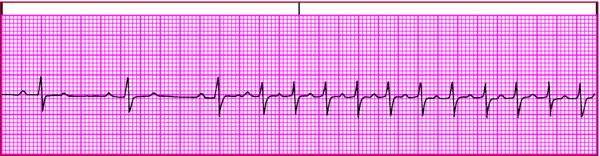
P wave - Abnormal, possibly hidden in previous T wave
QRS complex - Possibly aberrantly conducted
Other - One P wave for each QRS complex
|