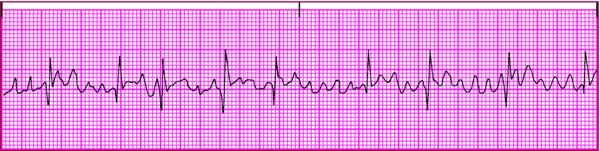
Distinguishing atrial fibrillation from atrial flutter It isn't uncommon for atrial flutter to have an irregular pattern of impulse conduction to the ventricles. In some leads, this pattern may be confused with atrial fibrillation. Here's how to tell the two arrhythmias apart. Atrial fibrillation 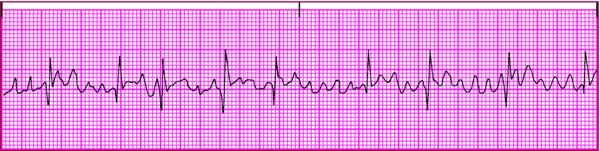
- Remember that fibrillatory waves (f waves) occur in an irregular pattern, making the atrial rhythm irregular.
- If you see atrial activity on the rhythm strip that, in some places, looks like flutter waves and seems to be regular for a short time and, in other places, looks like fibrillatory waves, interpret the rhythm as atrial fibrillation. Coarse fibrillatory waves sometimes have the characteristic sawtooth appearance of flutter waves.
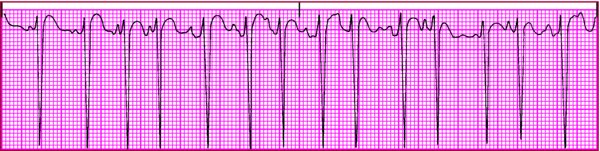
Atrial flutter 
- Look for characteristic abnormal P waves that produce a sawtooth appearance, known as flutter waves (F waves). These can be identified most easily in leads I, II, and V1.
- Remember that the atrial rhythm is regular. You should be able to map the F waves across the rhythm strip. Although some F waves may occur within the QRS or T waves, other F waves are visible and occur on time.
|