- Also known as ventricular escape rhythm, they are the rhythm of last resort
- Acts as safety mechanism to prevent ventricular standstill (asystole) when no impulses are conducted to the ventricles from above the bundle of His
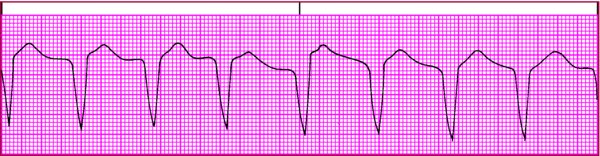
- The cells of the His–Purkinje system take over and act as the heart's pacemaker to generate electrical impulses with an inherent firing rate of usually 20 to 40 beats/min
- Idioventricular rhythms can occur as ventricular escape beats, idioventricular rhythm, or accelerated idioventricular rhythm
- They occur when all the heart's other pacemakers have failed or when supraventricular impulses can't reach the ventricles due to a block in the conduction system
- When the rate of an ectopic pacemaker site in the ventricles is less than 100 beats/min but exceeds the inherent ventricular escape rate of 20 to 40 beats/min, the rhythm is referred to as accelerated idioventricular rhythm (it's usually related to enhanced automaticity of ventricular tissue and has the same ECG characteristics as idioventricular rhythm except for heart rate)