A Look at Junctional Arrhythmias
Junctional arrhythmias originate in the atrioventricular (AV) junction—the area around the AV node and the bundle of His. The arrhythmias occur when the sinoatrial (SA) node, a higher pacemaker, is suppressed and fails to conduct impulses or when a block occurs in conduction. Electrical impulses may then be initiated by pacemaker cells in the AV junction.
Just Your Normal Impulse

In normal impulse conduction, the AV node slightly slows transmission of the impulse from the atria to the ventricles, giving the atria time to contract and pump as much blood as they can into the ventricles before the ventricles contract. However, impulses aren’t always conducted normally. (See Conduction in Wolff–Parkinson–White syndrome.)
| Now I get it! |
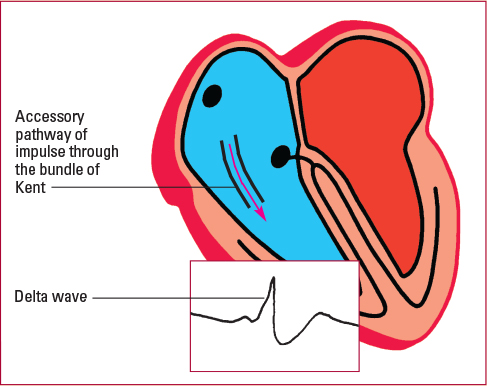
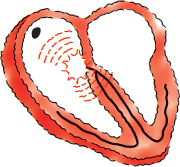
| Conduction in Wolff–Parkinson–White syndrome Conduction doesn’t always take place in a normal way. In Wolff–Parkinson–White syndrome, for example, an extra conduction pathway develops outside the AV junction and connects the atria with the ventricles, as shown. Wolff–Parkinson–White syndrome is typically a congenital rhythm disorder that occurs mainly in young children and adults of ages 20 to 35.
Rapidly Conducted The bypass formed in Wolff–Parkinson–White syndrome, known as the bundle of Kent, conducts impulses to the atria or the ventricles. Impulses aren’t delayed at the AV node, so conduction is abnormally fast. Retrograde conduction, circus reentry, and reentrant tachycardia can result in conduction pathways that interfere with each other, causing dizziness and syncope, palpitations, shortness of breath, and even cardiac arrest. Checking the ECG This syndrome causes a shortened PR interval (<0.10 second) and a widened QRS complex (>0.10 second). The beginning of the QRS complex may look slurred because of altered ventricular depolarization. This hallmark sign of Wolff–Parkinson–White syndrome is called a delta wave, shown in the inset. When to Treat This syndrome must be treated if tachyarrhythmias, such as atrial fibrillation and atrial flutter, occur. First, electrophysiology studies are done to determine the location of the conduction pathway and evaluate specific treatments. Radiofrequency ablation may be used with tachyarrhythmias that are resistant to medications such as adenosine or amiodarone. |
Which Way Did the Impulse Go?
Because the AV junction is located in the lower part of the right atrium near the tricuspid valve, impulses generated in this area cause the heart to be depolarized in an abnormal way. The impulse moves upward and causes backward, or retrograde, depolarization of the atria. P waves might not be seen, but if they are, look for them to be inverted in leads II, III, and aVF, leads in which you would normally see upright P waves. (See Finding the P wave)
| Mixed signals |
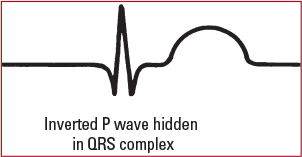
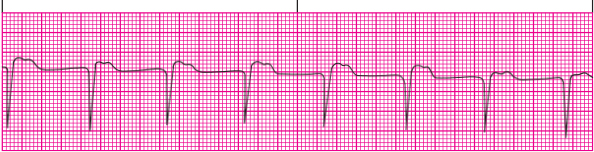
When the pacemaker fires in the AV junction, the impulse may reach either the atria or the ventricles first. Therefore, the inverted P wave and the following QRS complex won’t have a consistent relationship. These rhythm strips show the various positions the P wave can take in junctional rhythms. Atria First If the atria are depolarized first, the P wave will occur before the QRS complex.
Ventricles First If the ventricles are depolarized first, the QRS complex will come before the P wave.
Simultaneous If the ventricles and atria are depolarized simultaneously, the P wave will be hidden in the QRS complex.
|
The impulse also moves down toward the ventricles, causing forward, or antegrade, depolarization of the ventricles and an upright QRS complex. As this is the normal conduction pathway to, and through, the ventricles, the QRS complex has a normal configuration and duration and the T wave and QT interval are usually normal.

Junctional Mimic
Atrial arrhythmias are sometimes mistaken for junctional arrhythmias because impulses are generated so low in the atria that they cause retrograde depolarization and inverted P waves. Looking at the PR interval will help you determine whether an arrhythmia is atrial or junctional.
An arrhythmia with an inverted P wave before the QRS complex and a normal PR interval (0.12 to 0.20 second) originated in the atria. An arrhythmia with a PR interval less than 0.12 second originated in the AV junction.
Premature Junctional Contraction
A premature junctional contraction (PJC) is a beat that occurs before a normal beat and causes an irregular rhythm. This ectopic beat occurs when an irritable location within the AV junction acts as a pacemaker and fires either prematurely or out of sequence.
As with all beats produced by the AV junction, the atria are depolarized in a retrograde fashion, causing an inverted P wave. The ventricles are depolarized normally.
To help you remember what a PJC is, think of “beat before” for premature, “normal beat” for junctional, and “causing irregular rhythm” for contraction. |
How It Happens
PJCs may be caused by certain medications. An example is toxic levels of digoxin (level >2.5 mg/mL). They may also occur with excessive caffeine intake, inferior wall myocardial infarction (MI), electrolyte imbalances, hypothyroidism, rheumatic heart disease, valvular disease, hypoxia, heart failure, swelling of the AV junction after heart surgery, or other causes of inflammation or ischemia.
The Beat Goes on
Although PJCs themselves usually aren’t dangerous, you’ll need to monitor the patient carefully and assess him or her for other signs of intrinsic pacemaker failure.
What to Look for

A PJC appears on a rhythm strip as an early beat causing an irregularity. The rest of the strip may show regular atrial and ventricular rhythms, depending on the patient’s underlying rhythm.
P-Wave Inversion
Look for an inverted P wave in leads II, III, and aVF. Depending on when the impulse occurs, the P wave may fall before, during, or after the QRS complex. (See Identifying a PJC) If it falls during the QRS complex, it’s hidden. If it comes before the QRS complex, the PR interval is less than 0.12 second.
Because the ventricles are usually depolarized normally, the QRS complex has a normal configuration and a normal duration of less than 0.12 second. The T wave and the QT interval are usually normal.
That Quickening Feeling
The patient may be asymptomatic or may complain of palpitations or a feeling of quickening in the chest. You may be able to palpate an irregular pulse. If the PJCs are frequent enough, the patient may have hypotension from a transient decrease in cardiac output.
How You Intervene
Evaluation always includes vital signs and assessing the patient’s medication list, in addition to monitoring the ECG. PJCs usually don’t require treatment unless symptoms occur. In those cases, the underlying cause should be treated. If digoxin toxicity is the culprit, the medication should be discontinued and serum digoxin (Lanoxin) levels monitored.
You should also monitor the patient for hemodynamic instability. If ectopic beats are frequent, the patient should decrease or eliminate his or her caffeine intake.
A junctional escape rhythm is a string of beats that occur after a conduction delay from the atria. The normal intrinsic firing rate for cells in the AV junction is 40 to 60 beats/min.
Remember that the AV junction can take over as the heart’s pacemaker if higher pacemaker sites slow down or fail to fire or conduct. The junctional escape beat is an example of this compensatory mechanism. Because junctional escape beats prevent ventricular stand still, they should never be suppressed.
Backward and Upside Down
In a junctional escape rhythm, as in all junctional arrhythmias, the atria are depolarized by means of retrograde conduction. The P waves are inverted, and impulse conduction through the ventricles is normal. (See Check age and lifestyle.)
How It Happens
A junctional escape rhythm can be caused by any condition that disturbs SA node function or enhances AV junction automaticity. Common causes of the arrhythmia include:
- sick sinus syndrome
- vagal stimulation
- electrolyte imbalances
- digoxin toxicity
- inferior wall MI
- rheumatic heart disease
- chest trauma
- intracranial hemorrhage.
The Great Escape
Whether junctional escape rhythm harms the patient depends on how well the patient’s heart tolerates a decreased heart rate and decreased cardiac output. The less tolerant the heart is, the more significant the effects of the arrhythmia.

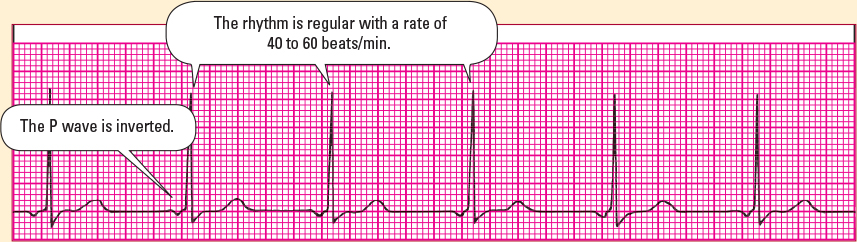
What to Look for
A junctional escape rhythm shows a regular rhythm of 40 to 60 beats/min on an ECG strip. Look for inverted P waves in leads II, III, and aVF.
The P waves occur before, after, or hidden within the QRS complex. The PR interval is less than 0.12 second and is measurable only if the P wave comes before the QRS complex. (See Identifying junctional escape rhythm.)
The rest of the ECG waveform—including the QRS complex, T wave, and QT interval—should appear normal because impulses through the ventricles are usually conducted normally.
It May Be Slow, but at Least It’s Regular
A patient with a junctional escape rhythm has a slow, regular pulse rate of 40 to 60 beats/min. The patient may be asymptomatic. However, pulse rates less than 60 beats/min may lead to inadequate cardiac output, causing hypotension, syncope, or decreased urine output.
How You Intervene
Treatment for a junctional escape rhythm involves correcting the underlying cause—for example, digoxin may be withheld. Atropine may be given to stimulate the sympathetic nervous system and increase the heart rate, or a temporary or permanent pacemaker may be inserted if the patient remains symptomatic.
Nursing care includes monitoring the patient’s serum digoxin and electrolyte levels and watching for signs of decreased cardiac output, such as hypotension, syncope, or decreased urine output. If the patient is hypotensive, lower the head of his or her bed as far as he or she can tolerate it and keep atropine at the bedside. Discontinue digoxin if indicated.

An accelerated junctional rhythm is caused by an irritable focus in the AV junction that speeds up to take over as the heart’s pacemaker. The atria are depolarized by means of retrograde conduction, and the ventricles are depolarized normally. The accelerated rate is usually between 60 and 100 beats/min.
How It Happens
Conditions that affect SA node or AV node automaticity can cause accelerated junctional rhythm. These conditions include:
- digoxin toxicity
- hypokalemia
- hypercalcemia
- inferior or posterior wall MI
- rheumatic heart disease
- valvular heart disease.
Getting a Kick Out of It
This arrhythmia is significant if the patient has symptoms of decreased cardiac output—hypotension, syncope, and decreased urine output. These symptoms can occur if the atria are depolarized after the QRS complex, which prevents blood ejection from the atria into the ventricles, or atrial kick.
What to Look for
With an accelerated junctional rhythm, look for a regular rhythm and a rate of 60 to 100 beats/min. (See Identifying accelerated junctional rhythm) If the P wave is present, it will be inverted in leads II, III, and aVF and will occur before or after the QRS complex or be hidden in it. If the P wave comes before the QRS complex, the PR interval will be less than 0.12 second. The QRS complex, T wave, and QT interval all appear normal. (See Escape rate higher in young children.)
Low-Down, Dizzy, and Confused
The patient may be asymptomatic because accelerated junctional rhythm has the same rate as sinus rhythm. However, the atria may not be able to fill completely before contracting or may not be able to empty sufficiently into the ventricles, lowering the cardiac output. The patient may become dizzy, hypotensive, and confused and have weak peripheral pulses.
How You Intervene
Treatment for accelerated junctional arrhythmia involves correcting the underlying cause. Nursing interventions include observing the patient to see how well he or she tolerates this arrhythmia, monitoring the serum digoxin level, and withholding the digoxin dose as ordered.
You should also assess potassium and other electrolyte levels and administer supplements as ordered, monitor vital signs for hemodynamic instability, and observe for signs of decreased cardiac output. Temporary pacing may be necessary if the patient is symptomatic.

In junctional tachycardia, three or more PJCs occur in a row. This supraventricular tachycardia occurs when an irritable focus from the AV junction has enhanced automaticity, overriding the SA node to function as the heart’s pacemaker.
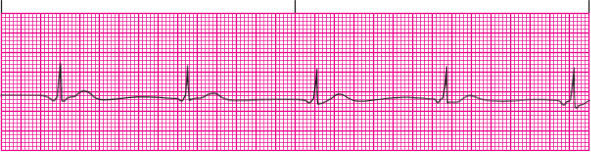
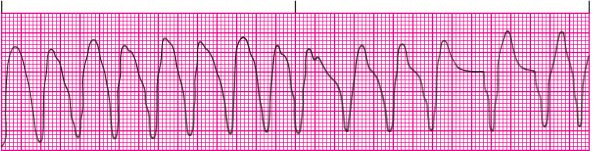
In this arrhythmia, the atria are depolarized by means of retrograde conduction, and conduction through the ventricles is normal. The rate is usually 100 to 200 beats/min. (See Identifying junctional tachycardia.)
How It Happens
Possible causes of junctional tachycardia include:
- digoxin toxicity (most common cause), which can be enhanced by hypokalemia
- inferior or posterior wall MI or ischemia
- congenital heart disease in children
- irritation and swelling of the AV junction after heart surgery.
Compromisin’ Rhythm
The significance of junctional tachycardia depends on the rate, underlying cause, and severity of the accompanying cardiac disease. At higher ventricular rates, junctional tachycardia may compromise cardiac output by decreasing the amount of blood filling the ventricles with each beat or atrial kick.
What to Look for
When assessing a rhythm strip for junctional tachycardia, look for a rate of 100 to 200 beats/min. The P wave is inverted in leads II, III, and aVF and can occur before, during (hidden P wave), or after the QRS complex.
Measurement of the PR interval depends on whether the P wave falls before, in, or after the QRS complex. If it comes before the QRS complex, the only time the PR interval can be measured, it will always be less than 0.12 second.
The QRS complexes look normal, as does the T wave, unless a P wave occurs in it or the rate is so fast that the T wave can’t be detected. (See Junctional and supraventricular tachycardia.)
Rapid Rate = Instability
Patients with rapid heart rates may have decreased cardiac output and hemodynamic instability. The pulse will be rapid, and dizziness, low blood pressure, and other signs of decreased cardiac output may be present.
How You Intervene
The underlying cause should be treated. If the cause is digoxin toxicity, the digoxin should be discontinued. Vagal maneuvers and medications such as IV adenosine may slow the heart rate for the symptomatic patient. Oral diltiazem may also be used along with a beta-blocker. (See Comparing junctional rates.)
If the patient recently had a MI or heart surgery, he may need a temporary pacemaker to reset the heart’s rhythm or until the irritation resolves and the heart tissue returns to normal. A child with a permanent arrhythmia may be resistant to drug therapy and require surgery. The patient with recurrent junctional tachycardia may be treated with ablation therapy, followed by permanent pacemaker insertion.
Monitor patients with junctional tachycardia for signs of decreased cardiac output. You should also check serum digoxin and potassium levels and administer potassium supplements, as ordered. If symptoms are severe and digoxin is the culprit, the practitioner may order digoxin immune fab, a digoxin-binding drug.