Drug interactions with alcohol are complex. Many patient-related and drug-related factors need to be considered. It can be difficult to predict outcomes accurately because a number of processes may occur simultaneously or consecutively.
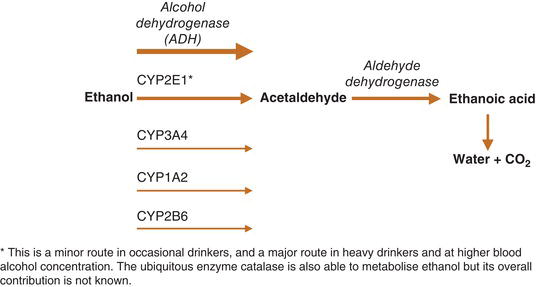
Alcohol (ethanol) is absorbed from the gastrointestinal tract and distributed in body water. The volume of distribution is smaller in women and the elderly where plasma levels of alcohol will be higher than in young males for a given intake of alcohol. Ingested alcohol is subject to metabolism by alcohol dehydrogenase (ADH). A small proportion of alcohol is metabolised by ADH in the stomach. The remainder is metabolised in the liver by ADH, and by CYP2E1. At low alcohol concentrations only ADH is active; CYP2E1 only begins to contribute when concentrations approach the legal driving limit of many countries (0.08%).5 CYP2E1 plays a minor role in occasional drinkers but is an important and inducible metabolic route in chronic, heavy drinkers. The induction of CYP2E1 accounts for the apparent tolerance of alcohol in heavy drinkers.6 CYP1A2, CYP3A4 and many other CYP enzymes also play a minor role in the metabolism of ethanol.7, 8
CYP2E1 and ADH convert alcohol to acetaldehyde. This is both the toxic substance responsible for the unpleasant symptoms of the ‘Antabuse reaction' (e.g. flushing, headache, nausea, malaise) and the compound implicated in hepatic damage. It may have psychotropic effects - ethanol is metabolised to acetaldehyde by CYP2E1 in the brain.9 The enzyme catalase is also known to metabolise alcohol to acetaldehyde in the brain and elsewhere.10 Acetaldehyde is further metabolised by aldehyde dehydrogenase to acetic acid and then to carbon dioxide and water (Figure ).
All of the enzymes involved in the metabolism of alcohol exhibit genetic polymorphism. For example, the majority of people of north Asian origin are poor metabolisers via aldehyde dehydrogenase.11 Enzyme function can change in response to alcohol. Chronic consumption of alcohol induces CYP2E1 and CYP3A4. The effects of alcohol on other hepatic metabolising enzymes have been poorly studied.
Table 11.8 lists drugs that inhibit ADH and aldehyde dehydrogenase.
Table 11.8 Drugs that Inhibit Alcohol Dehydrogenase and Aldehyde Dehydrogenase.
| Enzyme | Inhibited by | Potential consequences |
|---|---|---|
| Alcohol dehydrogenase | Aspirin H2 antagonists | Reduced metabolism of alcohol resulting in higher plasma levels for longer periods of time |
| Aldehyde dehydrogenase | Chlorpropamide Disulfiram Griseofulvin Isoniazid Isosorbide dinitrate Nitrofurantoin Sulphamethoxazole Tolbutamide | Reduced ability to metabolise acetaldehyde leading to ‘Antabuse' type reaction: facial flushing, headache, tachycardia, nausea and vomiting, arrhythmias and hypotension |
Interactions are difficult to predict in alcohol misusers because two opposing processes may be at work: competition for enzymatic sites during periods of consumption/intoxication (increasing drug plasma levels) and enzyme induction prevailing during periods of sobriety (reducing drug plasma levels10). In chronic drinkers, particularly those who binge-drink, blood levels of prescribed drugs may reach toxic levels during periods of intoxication with alcohol and then be sub-therapeutic when the patient is sober. Even in non-intoxicated individuals there is some evidence that co-administered alcohol confers competitive inhibition of CYP3A4, leading to increased exposure to drugs metabolised by this enzyme (Table 11.9).15 This makes it very difficult to optimise treatment of physical or mental illness.
Table 11.9 Co-Administration of Alcohol and Substrates for CYP2E1 and CYP3A4.5616
Substrates for enzyme (note: this is not an exhaustive list) | Effects in an intoxicated patient | Effects in a chronic, sober drinker | |
|---|---|---|---|
| CYP2E1 | Isoniazid Paracetamol Phenobarbitone Warfarin Zopiclone | Competition between alcohol and drug leading to reduced rates of metabolism of both compounds. Increased plasma levels may lead to toxicity | Activity of CYP2E1 is increased up 10-fold Increased metabolism of drugs potentially leading to therapeutic failure |
| CYP3A4 | Alprazolam Aripiprazole Benzodiazepines Carbamazepine Clozapine Donepezil Galantamine Haloperidol Methadone Mirtazapine Quetiapine Risperidone Sildenafil Tricyclics Valproate Venlafaxine Z-hypnotics | Competition between alcohol and drug leading to reduced rates of metabolism of both compounds. Increased plasma levels may lead to toxicity | Increased rate of drug metabolism potentially leading to therapeutic failure Enzyme induction can last for several weeks after alcohol consumption ceases |
Interactions of uncertain aetiology include increased blood alcohol concentrations in people who take verapamil and decreased metabolism of methylphenidate in people who consume alcohol. Alcohol may also, via various routes, impair the function of slow-release tablet mechanisms causing dose-dumping.17
Alcohol enhances inhibitory neurotransmission at gamma-aminobutyric acid A (GABA-A) receptors and reduces excitatory neurotransmission at glutamate N-methyl-D-aspartate (NMDA) receptors. It also increases dopamine release in the mesolimbic pathway and may have some effects on serotonin and opiate pathways. Given these actions, alcohol would be expected to cause sedation, amnesia and ataxia (Table 11.10) and give rise to feelings of pleasure (and/or worsen psychotic symptoms in vulnerable individuals).
Table 11.10 Pharmacodynamic Interactions with Alcohol.
| Effect of alcohol | Effect exacerbated by | Potential consequences |
|---|---|---|
| Sedation | Other sedative drugs, e.g.: Antihistamines Antipsychotics Baclofen Benzodiazepines Lofexidine Opiates Tizanidine Tricyclics Z-hypnotics | Increased CNS depression ranging from increased propensity to be involved in accidents through to respiratory depression and death |
| Amnesia | Other amnesic drugs, e.g.: Barbiturates Benzodiazepines Z-hypnotics | Increased amnesic effects ranging from mild memory loss to total amnesia. Usually anterograde amnesia: loss of memory of events after the effects of alcohol begin |
| Ataxia | ACE inhibitors Beta-blockers Calcium channel blockers Nitrates Adrenergic alpha receptor antagonists, e.g.: Clozapine Risperidone Tricyclics | Increased unsteadiness and falls |
ACE, angiotensin-converting enzyme; CNS, central nervous system.
Alcohol can cause or worsen psychotic symptoms by increasing dopamine release in mesolimbic pathways. The effect of antipsychotic drugs may be competitively antagonised, rendering them less effective.
Electrolyte disturbances secondary to alcohol-related dehydration can be exacerbated by other drugs that cause electrolyte disturbances (e.g. diuretics). Heavy alcohol consumption can lead to hypoglycaemia in people with diabetes who take insulin or oral hypoglycaemics. Theoretically there is an increased risk of lactic acidosis in patients who take metformin with alcohol. Alcohol can also increase blood pressure.
Chronic alcohol drinkers are particularly susceptible to the gastrointestinal irritant effects of aspirin and non-steroidal anti-inflammatory drugs.
In the presence of pharmacokinetic interactions, pharmacodynamic interactions may be more marked. For example, in a chronic heavy drinker who is sober, enzyme induction will increase the metabolism of diazepam, which may lead to increased levels of anxiety (treatment failure). If the same patient becomes intoxicated with alcohol, the metabolism of diazepam will be greatly reduced as it will have to compete with alcohol for the metabolic capacity of CYP3A4. Plasma levels of alcohol and diazepam will rise (toxicity). As both alcohol and diazepam are sedative (via GABA-A affinity), loss of consciousness and respiratory depression may occur.
Table 11.11 lists drugs that are safe and those that should be avoided in patients who continue drinking.
Table 11.11 Psychotropic Drugs: Choice in Patients Who Continue to Drink.
| Safest choice | Best avoided | |
|---|---|---|
| Antipsychotics | Sulpiride and amisulpride Paliperidone, if depot required (non-sedative and renally excreted) | Very sedative antipsychotics such as chlorpromazine and clozapine |
| Antidepressants | SSRIs - citalopram, sertraline Potent inhibitors of CYP3A4 (fluoxetine, paroxetine) may decrease alcohol metabolism in chronic drinkers | TCAs, because impairment of metabolism by alcohol (while intoxicated) can lead to increased plasma levels and consequent signs and symptoms of overdose (profound hypotension, seizures, arrhythmias and coma) Cardiac effects can be exacerbated by electrolyte disturbances Combinations of TCAs and alcohol profoundly impair psychomotor skills Mirtazapine - often very sedative MAOIs, as can cause profound hypotension. Also potential interaction with tyramine-containing drinks which can lead to hypertensive crisis |
| Mood stabilisers | Valproate (where regulations allow) Carbamazepine Higher plasma levels achieved during periods of alcohol intoxication may be poorly tolerated | Lithium, because it has a narrow therapeutic index and alcohol-related dehydration and electrolyte disturbance can precipitate lithium toxicity |
Note: be aware of the possibility of hepatic failure or reduced hepatic function in chronic alcohol misusers. See ‘Hepatic impairment' in Chapter 8. Also note the risk of hepatic toxicity with some recommended drugs (e.g. valproate).
MAOIs, monoamine oxidase inhibitors; TCAs, tricyclic antidepressants.