Drug treatment is the mainstay of therapy for mania and hypomania. Both antipsychotics and mood stabilisers are effective (although the nomenclature here is unhelpful - most, possibly all, antipsychotics are anti-manic and most mood stabilisers reduce psychotic symptoms in mania). Sedative and anxiolytic drugs (e.g. benzodiazepines) may add to the effects of these treatments.
Drug choice is made difficult by the small number of direct comparisons, such that no one individual drug can be recommended over another on efficacy grounds. However, an early network meta-analysis1 suggested that olanzapine, risperidone, haloperidol and quetiapine had the best combination of efficacy and acceptability. Cochrane reviews suggested olanzapine is more effective than both lithium2 and valproate3 when used as monotherapy. Olanzapine may also be more effective than asenapine.4 A 2024 network meta-analysis concluded that tamoxifen was the most effective individual drug.5
The benefit of antipsychotic mood stabiliser combinations (compared with a mood stabiliser alone) is established for those relapsing while on mood stabilisers but less clear for those presenting on no treatment.6, 7, 8, 9, 10 The most common study design is for participants to be randomised to continued mood stabiliser alone (a treatment that allows the emergence of mania) or to the failed mood stabiliser with a (newly introduced) antipsychotic. Overall, combination treatment with an antipsychotic and a mood stabiliser is more effective and quicker to act than either individual drug used alone.5, 11 Most formal guidelines recommend drug combinations as the first choice in mania,12 although single drug treatment may be considered, at least initially, for people presenting on no prior treatment.
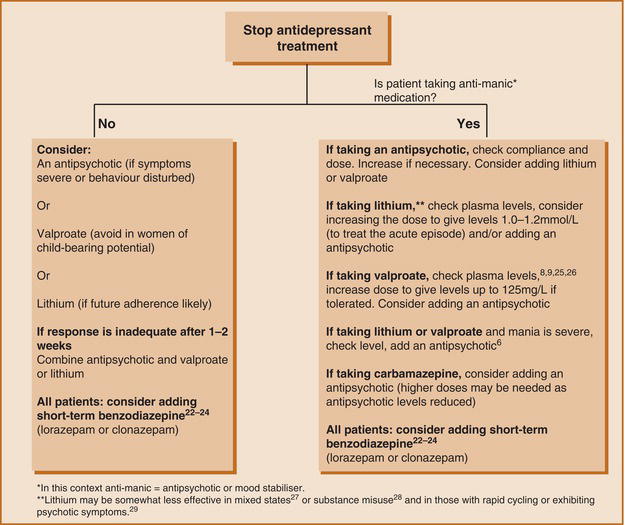
Figure outlines a treatment strategy for mania and hypomania. These recommendations are based on somewhat dated UK NICE guidelines,7 British Association for Psychopharmacology (BAP) guidelines32 and individual references cited in the diagram. Where an antipsychotic is recommended, choose from those licensed for mania/bipolar disorder (i.e. most conventional drugs, aripiprazole, asenapine, olanzapine, risperidone and quetiapine).
Figure. 2.7.1 Treatment of Acute Mania or Hypomania.
Valproate use is now heavily restricted, so lithium is likely to be the mood stabiliser most commonly used, at least in younger men and women. An alternative is carbamazepine, but this, like valproate, is teratogenic. Lamotrigine has no activity in mania33 and should not be used.
Suggested doses and alternative treatments are outlined in Tables 2.6 and 2.7.
Table 2.6 Mania: Suggested Drug Doses.
| Drug | Dose |
|---|---|
| Mood stabilisers | |
| Carbamazepine | 400mg MR twice daily increasing to 800-1600mg/day.3435 Dose may need to be increased after 2 weeks owing to induction of metabolism. |
| Lithium | 400mg/day, increasing every 3-4 days according to plasma levels. At least one study has used 800mg as a starting dose.36 |
| Valproate | As semi-sodium - 250mg three times daily increasing according to tolerability and plasma levels. Slow-release semi-sodium valproate may also be effective (at 15-30mg/kg)37 but there is one failed study.38 As slow-release sodium valproate - 500mg/day increasing as above. Higher, ‘loading doses' have been used, both oral394041 and intravenous.424344 The dose is 20-30mg/kg/day. |
| Antipsychotics | |
| Aripiprazole | 15mg/day increasing up to 30mg/day as required.45 Doses lower than 15mg may not be effective.46 |
| Asenapine | 5mg twice daily increasing to 10mg twice daily as required |
| Cariprazine | 3mg/day increasing up to 12mg a day as required47 |
| Olanzapine | 10mg/day increasing to 15 or 20mg as required |
| Risperidone | 2 or 3mg/day increasing to 6mg/day as required. The use of paliperidone in mania is not well supported.48 |
| Quetiapine | IR - 100mg/day increasing to 800mg as required. Higher starting doses have been used.49 XL - 300mg/day increasing to 600mg/day on day 2 |
| Haloperidol | 5-10mg/day increasing to 15mg if required |
| Benzodiazepines | |
| Lorazepam2526 | Up to 4mg/day (some centres use higher doses) |
| Clonzapam2426 | Up to 8mg/day |
Table 2.7 Mania: Other Possible Treatments.
| Treatment | Comments |
|---|---|
Allopurinol (300-600mg/day) | A meta-analysis of five studies of adjunct allopurinol found an effect size of just less than 0.3.50 |
Celecoxib (400mg/day)51 | Small RCT (n = 46) suggests benefit when used as adjunct to valproate. |
Clonidine (450-900mcg/day)52 | Limited data |
| Clozapine535455 | Established treatment option for refractory mania/bipolar disorder. Rapid titration has been reported.56 |
Endoxifen57 (4-8mg/day) | RCT evidence of efficacy. Major metabolite of tamoxifen. |
Gabapentin58 (up to 2.4g/day) | Probably only effective by virtue of an anxiolytic effect. Rarely used. Possibly useful as prophylaxis.59 |
Levetiracetam (up to 1500mg/day) | Effective as adjunctive treatment in two RCTs.6061 One case of levetiracetam causing mania.62 |
Melatonin (6mg/day)67 | Preliminary evidence of benefit as an adjunct to standard treatment. One small negative study.68 |
Memantine63 (10-30mg/day) | Conflicting evidence646566 |
(around 300-3000mg/day) | Probably effective acutely and as prophylaxis although one controlled study (conducted in youths) was negative.77 |
Phenytoin78 (300-400mg/day) | Rarely used. Limited data. Complex kinetics with narrow therapeutic range. |
Ritanserin79 (10mg/day) | Supported by a single RCT. Well tolerated. May protect against EPSEs. |
Tamoxifen80 (20-140mg/day) | Good evidence for efficacy as adjunct and as monotherapy, with large effect size. May provoke switch to depression. |
Topiramate81 (up to 300mg/day) | Probably not effective. Less effective than lithium.2 |
| Tryptophan depletion82 | Supported by a small RCT. |
| Ziprasidone838485 | Supported by three RCTs. Widely used outside UK. |
Entries are given in alphabetical order; no preference is implied by order in the table. Consult specialist and primary literature before using any treatment listed.
EPSEs, extrapyramidal side effects; RCT, randomised controlled trial.