AUTHOR: Adrienne B. Neithardt, MD
Spontaneous abortion is fetal loss before wk 20 of pregnancy, calculated from the patient’s last menstrual period, or the delivery of a fetus weighing <500 g. Early loss is before gestational age 12 6/7 wk, whereas late loss refers to losses from wk 13 to 20.1
Spontaneous abortion can also be classified as incomplete (partial passage of fetal tissue through partially dilated cervix), complete (spontaneous passage of all fetal tissue), threatened (uterine bleeding without cervical dilation or passage of tissue), inevitable (bleeding with cervical dilation without passage of fetal tissue), or missed abortion (intrauterine fetal demise without passage of tissue).
Recurrent spontaneous abortion involves three or more spontaneous pregnancy losses before wk 20. It affects approximately 1% of couples attempting to conceive. However, in actual practice, most reproductive experts consider two spontaneous pregnancy losses sufficient to initiate an evaluation for habitual or recurrent spontaneous abortion, since the risk of another loss is similar at this point, and the emotional stress is high. As many as 5% of couples and probably even a higher proportion of couples in which the woman is over age 35 are affected by two or more consecutive spontaneous abortions.2
| ||||||||||||
10% to 20% of clinically recognized pregnancies; 80% of miscarriages occur in the first trimester.1 Recurrent miscarriage occurs in <1% of couples attempting to have children.2
- Vaginal bleeding, which may have as high as a 50% chance of spontaneous abortion3
- Advancing maternal age
- Two or more prior miscarriages
- Significant underlying maternal health issues such as uncontrolled diabetes, thyroid disease, or other endocrine disturbances4
- Illicit substance use
- Obesity
- Alcohol, smoking, and excessive caffeine intake
- Use of fluconazole in pregnancy is associated with a statistically significant increased risk of spontaneous miscarriage5
- Fetal chromosomal aneuploidy and polyploidy account for the overwhelming majority of first-trimester losses.1,2,6
- Autosomal trisomy accounts for the majority of abnormalities, followed by monosomy X, tetraploidy, and, lastly, structural chromosomal abnormalities.6
- The incidence of trisomy increases as maternal age increases.1,6
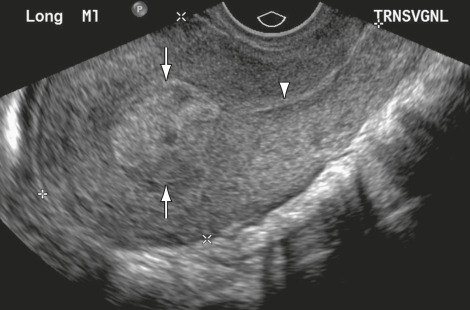
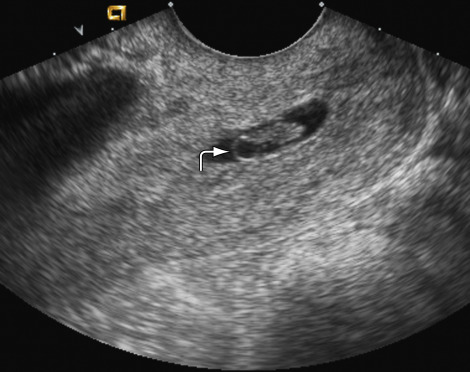
- Uterine anomalies: Müllerian abnormalities such as unicornuate, bicornuate, or septated uterus are associated with increased miscarriage risk, although rates vary in different studies. A septated uterus is most highly associated with recurrent loss and can be surgically corrected and thus is important to diagnose.7 Other intrauterine pathologies such as synechiae, leiomyomas, or prior DES exposure are important to rule out also.
- Incompetent cervix (iatrogenic or congenital, associated with 20% of midtrimester losses).
- Antiphospholipid antibody syndrome.
- Uncontrolled diabetes mellitus.4
- Rare or controversial causes include HLA associations between mother and father; infections such as tuberculosis, Chlamydia, and Ureaplasma; smoking and alcohol use; irradiation; progesterone deficiency; and environmental toxins. Most of the literature is observational in nature, which may skew risk factor data.2,4,5
- With two or more spontaneous miscarriages, a karyotype can be performed on the products of conception to evaluate for aneuploidy, which may be associated with a balanced translocation in one of the parents, and which has a substantially increased risk for abortion (depending on the actual type of translocation); if the pregnancy is carried to term, it has a 3% to 5% risk for an unbalanced karyotype.6 In patients with recurrent miscarriages, evaluation for anatomic defects such as uterine septum and for antiphospholipid syndrome (lupus anticoagulant, beta 2 glycoprotein IgG/IgM, and anticardiolipin antibody IgG/IgM) should also be obtained.2,4
- Profuse bleeding and cramping have a higher association with miscarriage than bleeding without cramping, which is more consistent with a threatened miscarriage.
- Cervical dilation with history or finding of fetal tissue at cervical os may be present.
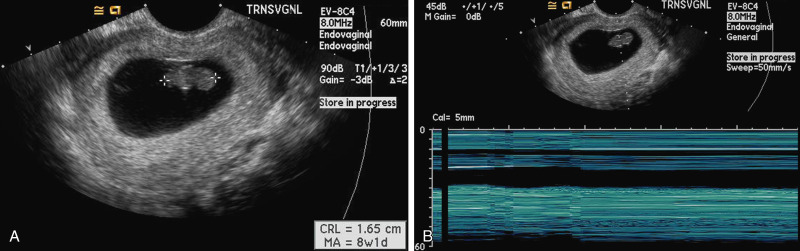
- In cases of missed abortion, uterine size may be smaller than menstrual dating, in contrast to molar gestation, where size may be greater than dates.
- The presence of nausea and vomiting in early pregnancy is associated with a reduced risk for pregnancy loss.8