AUTHOR: Fred F. Ferri, MD

DefinitionHidradenitis suppurativa (HS) is a chronic, relapsing suppurative cutaneous disease affecting skin that bears apocrine glands and is manifested by abscesses, fistulating sinus tracts, and chronic infection leading to scarring.
SynonymsAcne inversa
Apocrinitis
Verneuil disease
HS
| ICD-10CM CODE | | L73.2 | Hidradenitis suppurativa |
|
Epidemiology & DemographicsOnset is postpubertal, with an average age of onset of 23 yr; rates decline after age 55 yr.
PrevalenceOverall prevalence in the U.S. is ∼1% to 2%.
Predominant SexFemale:male ratio is 3:1.
Predominant AgeHS most often manifests after puberty, usually in the second or third decade of life. It is rare in the elderly.
Risk Factors
- Obesity and metabolic syndrome
- Family history (approximately 30%)
- Hyperandrogenism in women
- Cigarette smoking
Physical Findings & Clinical PresentationThe diagnosis is primarily clinical, based on the development of typical lesions in a characteristic distribution, with a relapsing nature. Early lesions are mainly painful “blind” boils, i.e., deep and rounded nodules. These may be transient and flare to become abscesses that either subside or transform into draining or nondraining tunnels. Gradually, postinflammatory scarring and tunnel formation occur in separate areas of the affected regions and ultimately coalesce to form stage III lesions. Early lesions can remit without treatment. Tunnels and scars are not generally amenable to medical treatment and thus indicate the need for surgical intervention. The course of HS is prolonged and marked by intermittent periods of activity and remission.
- Early symptoms include pain, itching, burning, erythema, and hyperhidrosis.
- Typical lesions include:
- Painful erythematous papules and nodules leading to painful abscesses with foul-smelling discharge
- Dermal contractures and rope-like elevation of the skin
- Comedones in the apocrine, gland-bearing skin
- Classified into Hurley Stages:
- Stage I: Abscesses without sinus tracts or scarring
- Stage II: Multiple abscesses plus sinus tracts and scarring
- Stage III: Diffuse involvement of entire area with abscesses, sinus tracts, and scarring
- The axilla is the most common site (Fig. E1).
- Less common sites include the inguinal region, the breasts (more often in women), and the perineal or perianal skin (more often in men).
- There is a strong tendency toward relapse and recurrence.
- There is often a poor response to conventional antibiotics and no pathogens isolated from cultures of lesions.
- The disease is often mistaken for a simple infection, and a long delay in diagnosis is common.
- Three clinical subtypes of HS have been recently proposed:
- A classic axillary-mammary HS subtype, representing 48% of cases and characterized by breast and axillary involvement and hypertrophic scarring.
- A follicular HS subtype, representing 26% of cases manifesting primarily in male smokers with a family history of HS and characterized by follicular lesions, including epidermal cysts, pilonidal sinus, comedones, and severe acne.
- A gluteal HS subtype, representing 26% of cases, most often seen in smokers with lower body mass index (BMI) and with a morphology characterized by follicular papules, folliculitis, and gluteal involvement.
Figure E1 Hidradenitis of the axilla.

From James WD et al: Andrews’ diseases of the skin: clinical dermatology, ed 12, Philadelphia, 2016, Elsevier.
Etiology
- Keratinous materials plug apocrine glands in hair follicles leading to stasis, dilation, rupture, and reepithelialization. Fig. E2 illustrates the pathogenesis of hidradenitis suppurativa.
- Bacteria are trapped and multiply, leading to gland rupture with surrounding inflammation and local bacterial infection.
- Over time, repeated nodules and infections cause scarring, which can lead to deep tissue damage and sinus tracts.
- Infectious agents such as Streptococcus, Staphylococcus, and Escherichia coli, and enteric flora have been identified in cultures but are likely a secondary component of the disease.
- There is likely a significant genetic component to the disease. 35% to 40% of patients report a family history of HS. An HS spectrum of different phenotypes has been characterized involving genetic factors that are not yet well described but may be important for future therapy.
- HS has been associated with other endocrine and autoimmune disorders such as diabetes, Cushing syndrome, acromegaly, Crohn disease, and inflammatory arthritis.
- Metabolic syndrome affects as many as 50% of patients with HS and may exacerbate the associated inflammation.
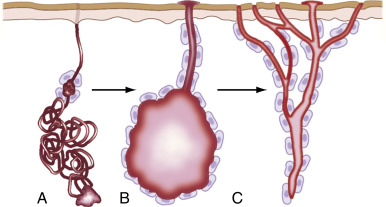
Figure E2 Pathogenesis of Hidradenitis Suppurativa, an Inflammatory Disease of the Apocrine Sweat Glands and Adjacent Connective Tissue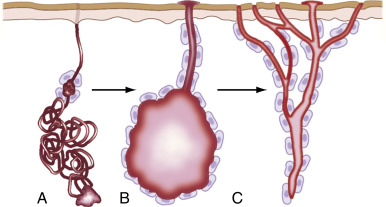
A, The initiating event is occlusion of the apocrine duct by a keratinous plug. B, Bacteria are trapped beneath the keratinous plug and multiply to form an abscess, which can rupture into adjacent tissue. C, The end result is recurrent abscesses, chronic draining sinuses, and indurated scarred skin and subcutaneous tissues. Often, multiple tracts are interconnected and lead to the skin.
From James WD et al: Andrews’ diseases of the skin, ed 12, Philadelphia, 2016, Elsevier.

There is no definitive cure for hidradenitis.
Nonpharmacologic Therapy
- Weight loss and control of metabolic syndrome
- Smoking cessation
- Avoidance of shaving, depilatory creams, deodorants
- Avoidance of tight-fitting clothing
- Warm compresses
- Incision and drainage of nonpurulent lesions is not recommended due to recurrence and scarring
- Laser therapy, radiotherapy, and cryotherapy currently under study
- Wide local excision for stage III disease with or without vacuum-assisted closure device
Acute & Chronic Rx1Current medical practice is mainly empirical. Several guidelines have been suggested for the management of HS. They all share the use of multimodal management, i.e., simultaneously using a three-pronged approach:
- Adjuvant therapy, which includes pain management, treatment of established superinfections, weight loss, and tobacco cessation. Treatment of superinfections is directed by bacterial culture sensitivities. Appropriate bandaging of suppurating lesions and patient support groups are helpful.
- Medical therapy, which may be topical in mild cases. Topical clindamycin has been shown to have an effect on early lesions. Resorcinol 15% BD can also be used as first-line treatment. Systemic tetracycline (500 mg BD) or doxycycline (100 mg BD) may be used as an alternative for severe/refractory disease. Cohort studies support coadministering oral clindamycin 300 mg BD and rifampicin 300 mg BD for limited HS. Smaller studies indicate that long-term intensive antibiotic treatment, e.g., the oral combination of rifampin (10 mg/kg once daily), moxifloxacin (400 mg once daily), and metronidazole (250-500 mg TD) (RMoM) for 6 wk, followed by 4 wk of RMo alone; cotrimoxazole after remission may provide long-term disease control in mild cases. Antibiotic resistance is frequent in the microbiota of HS patients and calls for more stringent antibiotic stewardship. For localized flares, intralesional corticosteroids (3-5 mg single dose) may provide significant pain relief within 24 hr.
Adalimumab has been shown to be effective in moderate-to-severe HS when administered weekly (week 0: 160 mg; week 2: 80 mg; and from week 4: 40 mg weekly). Onset of effect has been shown to be at week 2 of treatment. A post hoc analysis of a smaller trial indicated that infliximab 5 mg/kg may also be effective. Anakinra (100 mg daily) and apremilast (30 mg BD) may also be effective. An open-label study of ustekinumab (45 mg or 90 mg based on patient weight) also indicated utility.
Palliative medication includes systemic antiinflammatory drugs such as oral corticosteroid, dapsone, and ciclosporin. Patients may also benefit from acitretin 25 mg BD/TID, although this treatment is often limited by side effects and teratogenicity. HS shows little sign of improvement with isotretinoin. Hormonal therapy with cyproterone acetate may be helpful in some females but requires high and continued use, which raises safety concerns. A study found that spironolactone at doses ranging from 25 mg BD to 100 mg BD might be useful.
- Surgery, from local to extensive, can be helpful. Milder cases can benefit from localized excisions or deroofing (exteriorization) of single tunnels. Only fluctuant soft abscesses should undergo lancing. Lancing of inflamed nodules is painful to the patient, is ineffective, and causes additional scarring. Nonfluctuant symptomatic lesions are better treated using intralesional corticosteroids. A CO2 laser can be used to evaporate lesions. More advanced cases require major surgery, which should involve excision of the affected tissue or careful deroofing of all tunnels. The recurrence rate is inversely proportional to the extent of surgery, and wide excisions generally offer a better chance of remission. Similarly, it is suggested that secondary intention healing is superior to primary closure of postexcisional wounds. Secondary healing requires longer periods of wound management but generally does not preclude resumption of work 3 to 4 wk after treatment.
Complications
- Squamous cell carcinoma
- Scarring leading to restricted limb mobility or lymphedema
- Rectal or urethral fistulas
- Psychological effects related to disfiguring nature of disease
Referral
- Referral to dermatology during stage I to II disease.
- Referral to a surgeon is indicated for stage III disease.
- Surgical approaches include laser surgery and excisional surgery.