AUTHORS: Kelly C. Mead, MD and Manuel F. DaSilva, MD



DefinitionCompartment syndrome is a condition caused by elevated pressure within a confined myofascial space resulting in decreased perfusion, hypoxia, and eventual necrosis of the involved tissues. Acute compartment syndrome is a surgical emergency necessitating prompt diagnosis and intervention.
| ICD-10CM CODES: Code x Y (Y = encounter type: A (initial), D (subsequent), S (sequelae) | | T79.A0xA | Compartment syndrome, unspecified, initial encounter | | T79.A0xD | Compartment syndrome, unspecified, subsequent encounter | | T79.A0xS | Compartment syndrome, unspecified, sequelae | | T79.A19xY | Traumatic compartment syndrome of unspecified upper extremity | | T79.A11x Y | Traumatic compartment syndrome of the right upper extremity | | T79.A12x Y | Traumatic compartment syndrome of the left upper extremity | | T79.A29x Y | Traumatic compartment syndrome of unspecified lower extremity | | T79.A21x Y | Traumatic compartment syndrome of right lower extremity | | T79.A22x Y | Traumatic compartment syndrome of left lower extremity | | T79.A9x Y | Traumatic compartment syndrome of other sites | | M79.A19x Y | Nontraumatic compartment syndrome of unspecified upper extremity | | M79.A11x Y | Nontraumatic compartment syndrome of the right upper extremity | | M79.A12x Y | Nontraumatic compartment syndrome of the left upper extremity | | M79.A29x Y | Nontraumatic compartment syndrome of unspecified lower extremity | | M79.A21x Y | Nontraumatic compartment syndrome of right lower extremity | | M79.A22x Y | Nontraumatic compartment syndrome of left lower extremity | | M79.A9x Y | Nontraumatic compartment syndrome of other sites |
|
Epidemiology & Demographics
- Most commonly associated with acute trauma-related fractures (75% of cases)
- Tibial shaft most frequent fracture type (up to 10%), followed by distal radius fractures
- Other etiologies include soft tissue injuries, burns, vascular injuries, crush injuries, drug overdoses, reperfusion injuries, and bleeding diathesis
- Occurs more commonly among persons less than 35 yr old, with nearly 10 times higher incidence in males
Pathophysiology245Compartment syndrome occurs when elevated pressure within a myofascial compartment impairs blood flow and results in tissue ischemia and necrosis. As pressure within the anatomic compartment rises, it eventually exceeds the local capillary perfusion pressure resulting in capillary bed collapse. Venous outflow becomes compromised, leading to congestion and a subsequent decrease to the inflow of oxygenated blood. Hypoxia, ischemia, and cell death ensue. Decreased tissue perfusion can result in reversible neuropraxia within 1 h, myonecrosis, and other irreversible changes within 4 to 6 h.
A variety of clinical conditions are associated with the development of compartment syndrome and can be broadly categorized as conditions increasing fluid volume within the compartment, leading to significant soft tissue swelling, and decreasing volume of a compartment via external forces. Conditions that:
- Increase fluid volume within a compartment: Bleeding from a fracture, vascular injury, bleeding diathesis, and extravasation of intravenous fluids. Of note, it is possible to develop compartment syndrome even in the setting of an open fracture.
- Lead to significant soft-tissue swelling: Reperfusion injury, crush injury, high-energy soft-tissue injury (e.g., ballistic injury or severe contusion), thermal or electrical burn injuries, injection of recreational drugs, massive fluid resuscitation, and snake bites.
- Decrease the volume of a compartment via external forces: Tight external dressings (e.g., casts/splints), prolonged down time, or external pressure seen in anesthetized, sedated, or comatose patients who lie on an extremity for a prolonged period (e.g., drug overdose, intensive care unit (ICU) patients, and prolonged surgical procedures).
Physical Findings & Clinical Presentation6Clinical signs and symptoms of compartment syndrome include the five Ps as outlined here:
- Pain: Out of proportion for a given injury, or worsening pain despite adequate or escalating analgesia (earliest sign). Pain is often tested with passive stretch of the muscles within the compartment. Many trauma patients will complain of pain with any movement of the affected extremity. Therefore it may be useful for providers to attempt to distract patients while testing for pain with passive stretch.
- Paresthesia: Numbness or tingling in the sensory distribution of the nerve(s) traversing the compartment.
- Pulselessness: Late finding. Palpable peripheral pulses do not rule out compartment syndrome and may be present even in late stages of the disease due to collateral blood flow and reconstitution distal to the compartment of concern. Capillary refill can be sluggish or normal.
- Pallor: Late finding. Often secondary to compromised circulation within the affected extremity.
- Paralysis: Often a late finding. Low specificity and sensitivity for compartment syndrome as muscle weakness could be due to effort secondary to pain vs. true paralysis due to nerve and/or or muscle ischemia.
- Pediatric patients may demonstrate the three As: Agitation, Anxiety, and increasing Analgesia requirement.
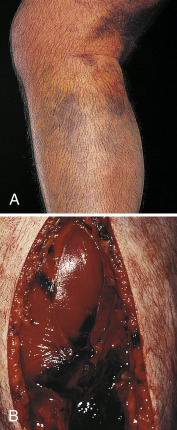
- Of note, health care workers performing a physical exam may palpate a tense or swollen compartment that is firm or noncompressible and “woodlike” (Fig. E1). However, studies have shown that manual detection of critical intracompartmental pressures is poor, even by experienced orthopedic surgeons, and therefore should only be used to raise suspicion for compartment syndrome.
Figure E1 A, Severe Calf Swelling Due to Anterior and Posterior Compartment Syndromes after Ischemia-ReperfusionB, Appearance after Emergency Fasciotomy. Note Edematous Muscle and Hematoma.
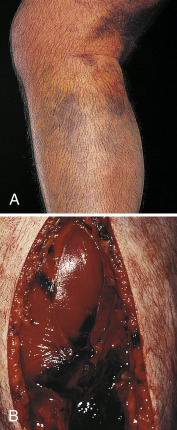
Courtesy Michael J. Allen, FRCS, Leicester, UK. From Floege J et al: Comprehensive clinical nephrology, ed 4, Philadelphia, 2010, Saunders.
 DIAGNOSIS4,6
DIAGNOSIS4,6Compartment syndrome is a clinical diagnosis based on history and examination. Acute compartment syndrome can develop quickly or evolve over time, and therefore serial examinations are critical. Typically, acute compartment syndrome will develop within 48 to 72 h of injury. The diagnosis may be confirmed with the use of intracompartmental pressure-measuring devices in the setting of unreliable, comatose, or otherwise nonresponsive patients.
 TREATMENT1-3,-6,8
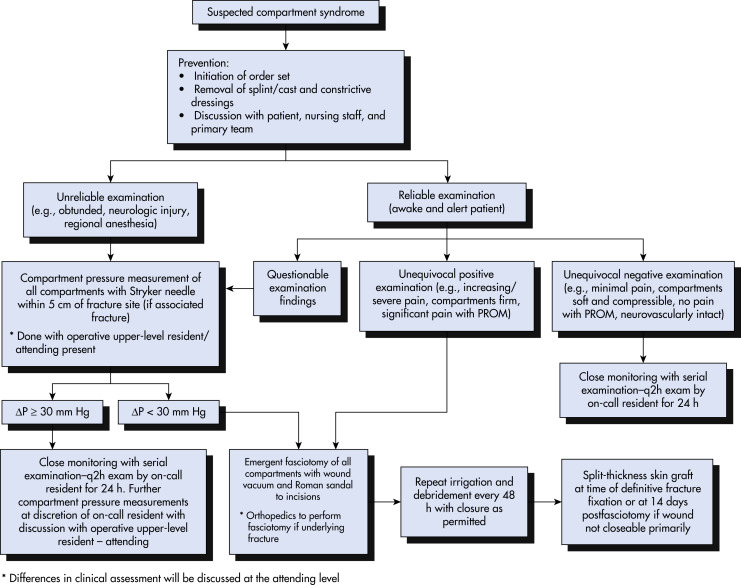
TREATMENT1-3,-6,8Treatment goal of fasciotomy is to reduce the intracompartmental pressure and prevent tissue ischemia and necrosis (Fig. E2).
FIG E2 Algorithm for the Management of a Patient with Suspected Compartment SyndromeProm, Passive Range of Motion.
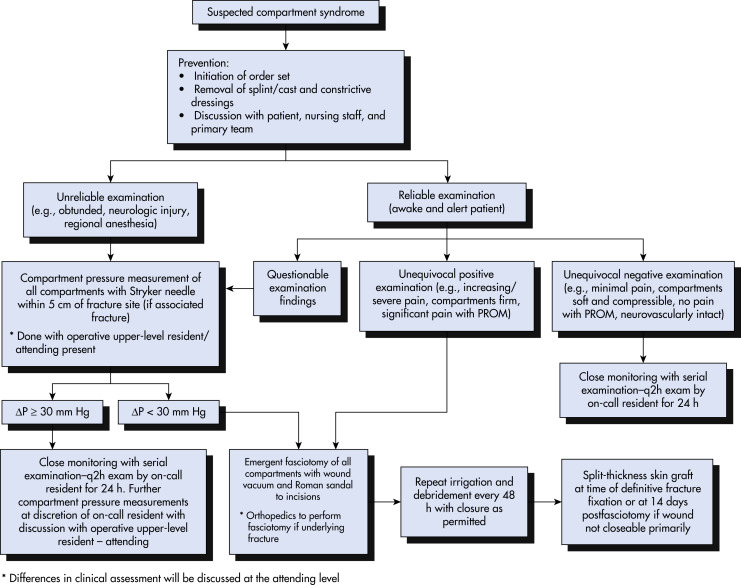
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.

- Compartment syndrome is a surgical emergency necessitating prompt diagnosis and intervention. It is commonly associated with fractures, most commonly tibial shaft and both bone forearm fractures.
- Compartment syndrome is a clinical diagnosis, and intracompartmental pressure measurements are not required to make or confirm the diagnosis.
- Pain out of proportion to an injury, pain with passive stretch, increasing analgesia requirements, progressive sensory or motor neurologic deficits, or changes in vascular/perfusion status should raise concern for compartment syndrome.
- The presence of palpable peripheral pulses does not rule out compartment syndrome.
- Patients receiving a cast to manage their fractures should be educated about the risk of swelling in addition to the signs and symptoms of compartment syndrome. Instructions should be provided to return to their casting provider and/or go to the nearest emergency department if these symptoms develop.
DIFFERENTIAL DIAGNOSIS- Physiologic soft-tissue edema or swelling
- Muscle strain or contusion
- Cellulitis
- Gangrene
- Peripheral vascular injury
- Necrotizing fasciitis
- Stress fracture
- Deep vein thrombosis and thrombophlebitis
- Tendinitis
- Tarsal tunnel or posterior ankle syndrome
- Popliteal artery impingement
- Claudication
- Tumor
- Venous insufficiency
LABORATORY TESTS7,8Laboratory values are not useful in the diagnosis of acute compartment syndrome, but are important for other diagnoses or associated conditions.
- International normalization ratio/prothrombin time (INR/PT) and partial thromboplastin time (PTT) to assess coagulation profile
- CBC with differential for evaluation of infection
- Creatine phosphokinase (CK) levels, which can rise as muscle injury develops (e.g., crush injury, rhabdomyolysis)
- Metabolic panel for the assessment of electrolytes and renal function
- Urinalysis for rhabdomyolysis
- Urine and serum myoglobin levels
IMAGING STUDIES- Radiographs of the affected extremity should be obtained to evaluate for fracture, foreign body, or other osseous and soft-tissue abnormalities.
- Ultrasonography or Doppler ultrasonography can be used to rule out deep vein thrombosis and evaluate blood flow to the extremity. Arteriography can be used to evaluate for arterial injury and blood flow within a compartment.
DIAGNOSTIC STUDIES2,3,6-8- Measuring direct intracompartmental pressure is an adjunct tool to aid in the diagnosis of compartment syndrome.
- Intracompartmental pressure measurement can be obtained using a handheld or simple needle manometer system, or using a wick or slit catheter.
- If intracompartmental pressure is ≥30 mm Hg or when the difference between diastolic blood pressure and compartment pressure (Δ pressure) is ≤30 mm Hg, a fasciotomy is indicated.
ACUTE GENERAL Rx- Analgesics for pain control.
- Advanced Trauma Life Support (ATLS) management, as hypotension can worsen tissue perfusion and ischemia.
- Remove circumferential dressings, casts, and all external pressure generators.
- The affected extremity should be elevated at or just above the level of the heart to aid in resolution of swelling. Excessive elevation can reduce limb perfusion.
- The standard of care is emergent fasciotomy and thorough débridement of nonviable tissue. Performance of fasciotomies more than 4 to 6 h after ischemia onset will most likely result in irreversible tissue necrosis.
- Measurement of compartment pressure is not necessary to confirm diagnosis, and fasciotomy should not be delayed in the setting of high clinical suspicion.
- Associated fractures should be stabilized with internal or external fixation to reduce further soft tissue injury.
CHRONIC Rx- Patients who display evidence of tissue necrosis should return to the operating room every 48 h to assess tissue viability and repeat debridement as needed.
- A negative pressure wound therapy system, wet-to-dry dressings, or other hemostatic dressings may be placed over fasciotomy wounds with delayed primary wound closure and skin grafting as needed.
- Negative pressure wound therapy systems should be avoided in patients with coagulopathy, or other significant risks for bleeding.
- Local wound care should be emphasized to decrease the risk of infection.
- Definitive closure of the soft-tissue envelope should be completed within approximately 7 days of fasciotomy.
DISPOSITIONWith early diagnosis and prompt intervention, the prognosis and functional outcomes are excellent. The following are sequelae of delayed or undiagnosed compartment syndrome:
- Myonecrosis
- Permanent nerve damage and paralysis
- Muscle contracture (e.g., Volkmann contracture in the forearm)
- Gangrene
- Infection and possible sepsis
- Amputation
- Rhabdomyolysis and possible renal failure
- Cardiac arrhythmias and possible death from reperfusion injury and electrolyte abnormalities
REFERRALPatients with suspected compartment syndrome should be promptly referred to an orthopedic and/or general surgeon knowledgeable in the performance of fasciotomies in the affected area.