AUTHOR: Danylo Zorin, MD
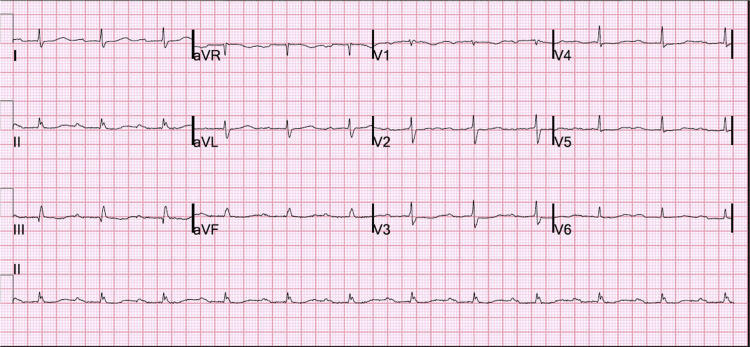
First-degree atrioventricular (AV) block is defined as a PR interval exceeding 200 msec with preserved 1:1 AV conduction relationship. AV block is actually a misnomer because every atrial impulse is conducted to ventricles, and some refer to this finding as first-degree AV delay.1,2
Atrioventricular conduction delay
| ||||||||
Based on studies conducted in healthy volunteers, the incidence varies between 5 and 10 in 1000.
Overall prevalence between 1% and 2% has been reported. It increases with age from ∼1% in young (20- to 30-yr-old) adults to ∼3% to 4% by age 60. In a cohort over age 60, prevalence is ∼6%.3
Age (more common with advanced age), male sex (men on average have longer PR intervals), race (African Americans tend to have longer PR intervals), family history, and comorbid conditions (e.g., hypertension, diabetes) are major risk factors.
Genome-wide association studies identified genes (e.g., SCN5A and more recently SCN10A, encoding voltage-gated sodium channel) that can determine PR interval duration.4
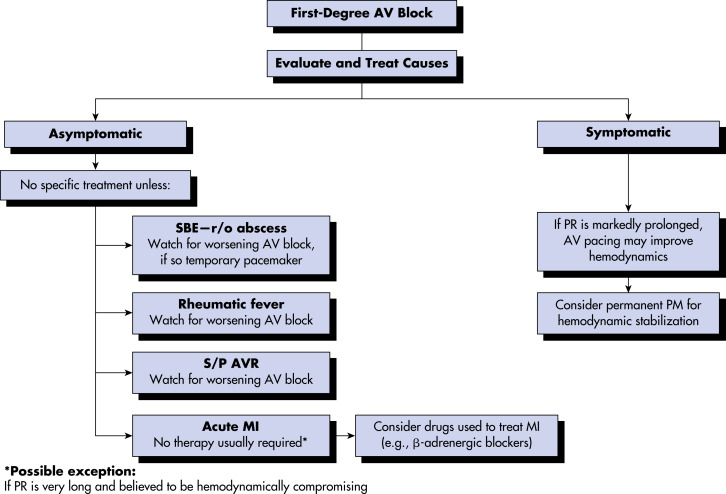
- Clinical presentation of a first-degree AV block depends on the duration of PR interval. Insignificant prolongation has no hemodynamic consequences and hence is asymptomatic. Progressive prolongation causes decrease in intensity of the S1 heart sound and sometimes its complete disappearance. This is due to premature partial or complete closure of atrioventricular valves caused by reverse diastolic ventriculoatrial pressure gradient, especially with decreased ventricular compliance.
- In some patients, diastolic mitral regurgitation can be demonstrated. Further lengthening of AV conduction time (particularly beyond 300 msec, termed marked first-degree AV block) causes “pseudopacemaker syndrome” when atria contract against closed atrioventricular valves due to encroachment of atrial systole on the previous ventricular systole. This leads to increased pressure in both atria, inferior vena cava, superior vena cava, and pulmonary veins, and loss of “atrial kick” with ensuing drop in end-diastolic volume, stroke volume, and cardiac output. Typical symptoms of the pseudopacemaker syndrome include malaise, poor exercise tolerance, dyspnea, orthopnea, cough, atypical chest discomfort, sensation of throat fullness, and occasionally presyncope or syncope.
- Physical examination may reveal hypotension, rales, increased jugular venous pressure with cannon A waves, peripheral edema, and murmurs of tricuspid and/or mitral regurgitation.1,5
Causes of AV block are numerous. They can be broadly divided into congenital and acquired. Acquired causes can in turn be broken down into infectious, inflammatory, degenerative, ischemic, vagotonic, metabolic, and iatrogenic. Congenital causes include conditions where a heart block is a part of a syndrome (such as myotonic dystrophy type 1, Emery-Dreifuss, limb-girdle type 1B) or a primary abnormality (as in familial Lev-Lenègre disease due to mutation of the SCN5A gene). A number of infections (Lyme disease, Chagas disease, toxoplasmosis), metabolic disorders (hyperkalemia, hypothyroidism), inflammatory conditions (systemic lupus erythematosus, rheumatoid arthritis, sarcoidosis), therapeutic interventions (beta-blockers, nondihydropyridine calcium channel blockers, valve surgeries, digoxin, etc.), toxins (CO, cyanide, mercury), degenerative processes (senile idiopathic fibrosis of the conduction system, aortic valve calcification), ischemia (acute myocardial infarction, chronic stable coronary artery disease), and increased vagal tone (in athletes or patients with sleep apnea) can be responsible for acquired AV block.1