AUTHOR: Glenn G. Fort, MD, MPH
Sinusitis is inflammation of the mucous membranes lining one or more of the paranasal sinuses. The various presentations are:
- Acute sinusitis: Infection lasting <4 wk, with complete resolution of symptoms.
- Subacute infection: Lasts from 4 to 12 wk, with complete resolution of symptoms.
- Recurrent acute infection: Episodes of acute infection lasting <30 days, with resolution of symptoms, which recur at intervals at least 10 days apart.
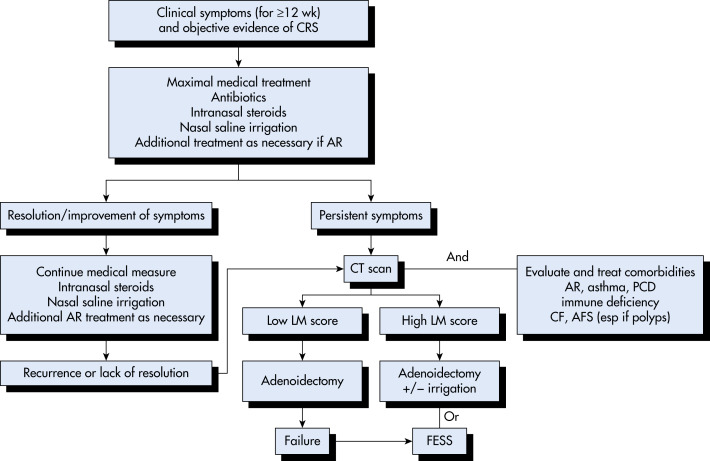
- Chronic sinusitis: Inflammation of the paranasal sinuses and nasal cavities lasting >12 wk, with persistent upper respiratory symptoms. It accounts for 1% to 2% of total physician encounters.
- Acute bacterial sinusitis superimposed on chronic sinusitis: New symptoms that occur in patients with residual symptoms from prior infection(s). With treatment, the new symptoms resolve, but the residual ones do not.
Rhinosinusitis: Sinusitis is almost always accompanied by inflammation of the nasal mucosa; thus it is now the preferred term.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Patients often give a history of a recent upper respiratory illness with some improvement, then a relapse.
- Mucopurulent secretions in the nasal passage:
- Erythema, swelling, and tenderness over the infected sinus in a small proportion of patients:
- Intermittent low-grade fever in about half of adults with acute bacterial sinusitis.
- Toothache is a common complaint when the maxillary sinus is involved.
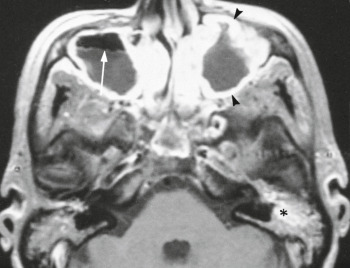
- Periorbital cellulitis and excessive tearing with ethmoid sinusitis:
- Characteristics of acute sinusitis in children with upper respiratory tract infections:
- Symptoms of chronic sinusitis (may or may not be present):
- Nosocomial sinusitis is typically seen in patients with nasogastric tubes or nasotracheal intubation.
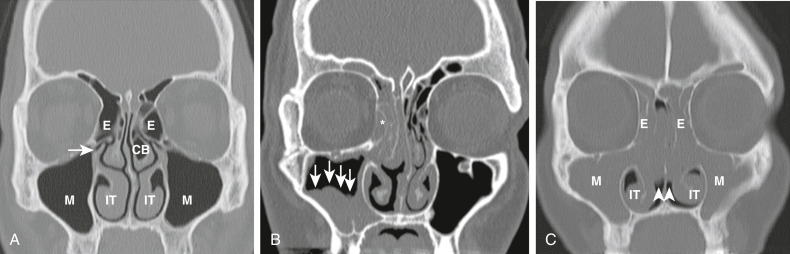
- Each of the four paranasal sinuses is connected to the nasal cavity by narrow tubes (ostia), 1 to 3 mm in diameter; these drain directly into the nose through the turbinates. The sinuses are lined with a ciliated mucous membrane (mucoperiosteum).
- Acute viral infection:
- Other predisposing factors:
- Dental infections lead to maxillary sinusitis.
- Viruses recovered alone or in combination with bacteria (in 16% of cases):
- The principal bacterial pathogens in sinusitis are Streptococcus pneumoniae, nontypable Haemophilus influenzae, and Moraxella catarrhalis (Table 1).
- In the remainder of cases Streptococcus pyogenes, Staphylococcus aureus, beta-hemolytic streptococci, and mixed anaerobic infections (Peptostreptococcus, Fusobacterium, Bacteroides, and Prevotella spp.) are found.
- Infection is polymicrobial in about one third of cases.
- Anaerobic infections are seen more often in cases of chronic sinusitis and in cases associated with dental infection; anaerobes are unlikely pathogens in sinusitis in children.
- Fungal pathogens are isolated with increasing frequency in immunocompromised patients but remain uncommon pathogens in the paranasal sinuses. Fungal pathogens include Phaeohyphomycosis, Aspergillus, Pseudallescheria, Sporothrix, and Zygomycetes spp.
- Nosocomial infections: Occur in patients with nasogastric tubes, nasotracheal intubation, cystic fibrosis, and immunocompromised state.
- Organisms typically isolated in chronic sinusitis:
TABLE 1 Microbiology of Acute Bacterial Rhinosinusitis in Adults
| Organism | Range of Prevalence (%) | ||
|---|---|---|---|
| Streptococcus pneumoniae | 20-43 | ||
| Haemophilus influenzae | 22-35 | ||
| Streptococcus spp | 3-9 | ||
| Anaerobes | 0-9 | ||
| Moraxella catarrhalis | 2-10 | ||
| Staphylococcus aureus | 0-8 | ||
| Other | 4 |
From Broaddus VC et al: Murray & Nadel’s textbook of respiratory medicine, ed 7, Philadelphia, 2022, Elsevier.