AUTHOR: Fred F. Ferri, MD
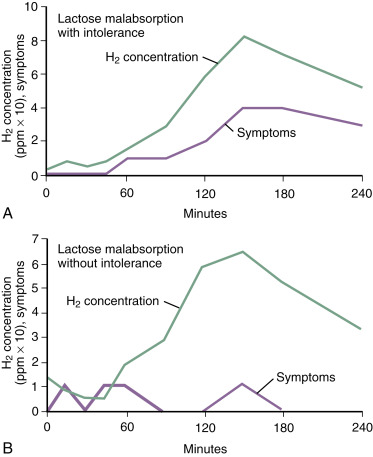
Lactose intolerance is the insufficient concentration of lactase enzyme, leading to fermentation of malabsorbed lactose by intestinal bacteria with subsequent production of intestinal gas and various organic acids, manifesting clinically with diarrhea, abdominal pain, flatulence, or bloating after lactose intake. Lactose malabsorption occurs when a substantial amount of lactose is not absorbed in the intestine. Lactase deficiency is defined as brush-border lactase activity that is markedly reduced relative to the activity observed in infants.
- Nearly 50 million people in the U.S. have partial or complete lactose intolerance. There are racial differences, with <25% of White adults being lactose intolerant but >85% of Asian Americans and >60% of African Americans having some form of lactose intolerance.
- There are geographic variations: Highest in Asians (up to 90%), lowest in northern Europeans (approximately 10%), intermediate in southern Europeans and Middle Eastern populations (up to 40%).
- Before it can be absorbed, lactose is cleared to glucose and galactose by the enzyme lactase in the brush border of the small intestine. If the amount of lactase is marginal or its expression is left, lactose intolerance will result.
- Congenital lactase deficiency: Common in premature infants; rare in term infants and generally inherited as a chromosomal recessive trait.
- Secondary lactose intolerance: Usually a result of injury of the intestinal mucosa (Crohn disease, viral gastroenteritis, AIDS enteropathy, cryptosporidiosis, Whipple disease, sprue).
- Acquired primary lactase deficiency (adult-type hypolactasia OMIM #223100) is the most common form of lactase deficiency worldwide. The decline in lactase activity is a multifactorial process that is regulated at the gene transcription level and leads to decreased biosynthesis, retardation of intracellular transport, or maturation of the enzyme lactase-phlorizin hydrolase.