AUTHOR: Fred F. Ferri, MD
Crohn disease (CD) is an inflammatory disease of the bowel of unknown etiology, most commonly involving the terminal ileum and manifesting primarily with diarrhea, abdominal pain, fatigue, and weight loss.
Inflammatory bowel disease (IBD)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Physical exam findings vary depending on disease location and severity
- Abdominal tenderness, mass, or distention
- Chronic or nocturnal diarrhea
- Weight loss, fever, night sweats
- Hyperactive bowel sounds in patients with partial obstruction, bloody diarrhea
- Delayed growth and failure of normal development in children
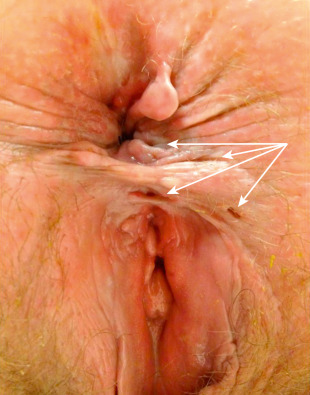
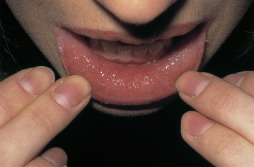
- Perianal and rectal abscesses, perianal fistulas (Fig. E1), anal tags (Fig. E2), multiple sinuses and scarring (Fig. E3), mouth ulcers, cobblestone appearance of oral mucosa (Fig. E4), and atrophic glossitis
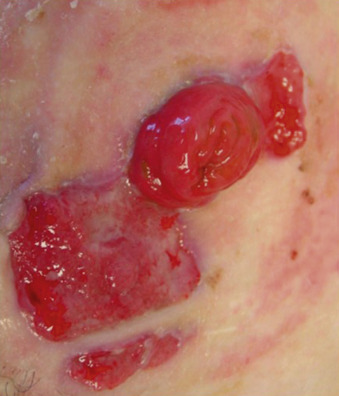
- Extraintestinal manifestations (Table E1): Joint swelling and tenderness, hepatosplenomegaly, erythema nodosum (Fig.E5), pyoderma gangrenosum (Fig. E6), clubbing, tenderness to palpation of the sacroiliac joints
- Symptoms may be intermittent, with varying periods of remission
- Overall, 45% to 50% of patients have ileocolonic inflammation, 30% have isolated small bowel disease, 20% have isolated colonic disease, and 5% have isolated upper GI or perianal manifestations
TABLE E1 Extraintestinal Manifestations of Inflammatory Bowel Disease
| Feature or Disease | Crohn | Ulcerative Colitis |
|---|---|---|
| Peripheral arthritis | ∼15% | ∼10% |
| Axial or sacroiliac arthritis | ∼15%-20% | ∼10%-15% |
| Septic arthritis | Rare | Not reported |
| Skin | ||
| Erythema nodosum | Up to 15% | <15% |
| Erythema multiforme | Rare | ? |
| Pyoderma gangrenosum | 0.5%-2% | 0.3%-0.4% in severe disease |
| Aphthous ulcers | Rare | 1%-8% |
| Nephrolithiasis (oxalate) | <15% | ? |
| Amyloidosis | Very rare | Not reported |
| Liver disease | 3%-5% | 7% |
| Uveitis | 13% | 4% |
| Vasculitis | Takayasu | <5% |
| Clubbing of fingers | Yes | 1%-5% |
| Increased prevalence of asthma | Yes | Yes |
| Increased prevalence of multiple sclerosis | No | Yes |
From Firestein GS et al: Kelly’s textbook of rheumatology, ed 9, Philadelphia, 2013, Saunders.
Note the Multiple External Fistula Openings Shown by the White Arrows. These All Had a Common Internal Opening in the Anterior Midline, Which was Also Associated with a Rectovaginal Fistula. This Patient Ultimately Elected to Undergo Ileostomy Diversion.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Note the Bluish Coloring and Waxy Appearance of the Perianal Skin.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
This Patient Had a Lesion of Pyoderma Gangrenosum When First Seen and Developed Inflammatory Plaques with the Appearance of Sweet Disease on the Trunk (with the Novel Feature of a Koebner Reaction into Recent Scars).
From White GM, Cox NH [eds]: Diseases of the skin: a color atlas and text, ed 2, St Louis, 2006, Mosby.
In This Fairly Quiescent Example, There is a Granular Cobblestoned Appearance. Some Patients have More Aggressive Fissured and Ulcerated Plaque Lesions.
From White GM, Cox NH [eds]: Diseases of the skin: a color atlas and text, ed 2, St Louis, 2006, Mosby.
Note the Red Purplish Nodule on the Dorsum of the Foot.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Here, the Lesions have Started to Heal with Granulation Tissue.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
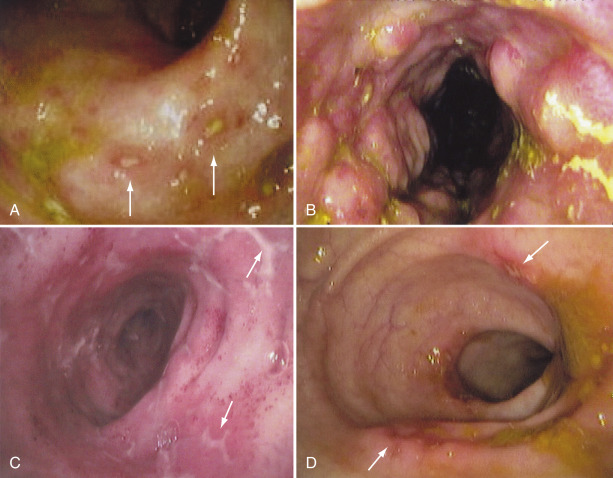
A Wide Variety of Findings May Be Visualized on Endoscopy, in Part Depending on the Duration and Severity of the Inflammation. A, Typical Aphthous Ulcers (Arrows) Consisting of a Central White Depression Surrounded by a Slightly Elevated, Erythematous Rim Only a Few Millimeters in Diameter. B, Findings More Typical of Advanced Disease, with Erythema, Edema, and a Cobblestone Appearance. C, Stellate Ulcers (Arrows) in the Terminal Ileum. D, Discrete Ulcers (Arrows) with Normal Intervening Mucosa Typical of the Patchy Inflammation Seen in Crohn Disease.
From Feldman M et al: Sleisenger and Fortran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.