AUTHORS: Jason Lin, BA and Edward J. Testa, MD
Calcium pyrophosphate dihydrate crystal deposition (CPPD) disease refers to the precipitation of calcium pyrophosphate dihydrate (CPP) in connective tissues that may be asymptomatic or may be associated with several clinical syndromes, including acute and chronic arthritis.1 CPP was formerly abbreviated and commonly referred to as “CPPD,” but the abbreviation is now reserved for “CPP deposition.” Alternative names (Table 1) representing specific clinical or radiographic features of CPPD disease include pseudogout, chondrocalcinosis, and pyrophosphate arthropathy.2
TABLE 1 Nomenclature of Calcium Pyrophosphate and Associated Syndromes
| Definition | Old Terms | EULAR Recommendations | Preferred Term (Abbreviation) |
|---|---|---|---|
| Radiographic correlate of CPPD | Chondrocalcinosis, chondrocalcinosis articularis | Chondrocalcinosis | Chondrocalcinosis (CC) |
| Acute inflammatory arthritis caused by CPP crystals | Pseudogout | Acute CPP crystal arthritis | Acute CPP crystal arthritis |
| Calcium pyrophosphate dihydrate crystals | Calcium pyrophosphate dehydrate; calcium pyrophosphate dihydrate | Calcium pyrophosphate crystals | Calcium pyrophosphate crystals (CPP crystals) |
| All clinical syndromes associated with CPP crystals | Calcium pyrophosphate dihydrate deposition disease | None | Calcium pyrophosphate deposition disease (CPPD) |
| Chronic arthritis caused by CPP crystals ± inflammation | Calcium pyrophosphate dihydrate deposition disease: Pyrophosphate arthropathy; pseudorheumatoid arthritis; pseudoosteoarthritis | Chronic CPP crystal arthritis, OA with CPPD | Chronic CPP crystal arthritis, OA with CPPD |
| Deposition of calcium pyrophosphate crystals in joints or tissue with or without clinical symptoms | Calcium pyrophosphate dihydrate deposition | CPPD | Calcium pyrophosphate deposition (CPPD) |
CPP, Calcium pyrophosphate; CPPD, calcium pyrophosphate dihydrate crystal deposition disease; EULAR, European League Against Rheumatism; OA, osteoarthritis.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
Pseudogout/acute CPP crystal arthritis is used to describe acute attacks of CPP crystal-induced arthritis that clinically resembles the arthritis that is commonly encountered in gout.3,4 The term acute CPP crystal arthritis is now preferred in place of pseudogout.
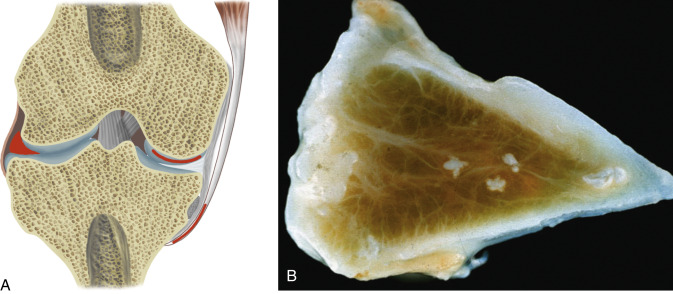
Chondrocalcinosis (CC) refers to radiographic calcification in hyaline cartilage and/or fibrocartilage and does not confirm the diagnosis of CPP-related arthritis as it can be present in other types of crystal deposition diseases or be asymptomatic.2,5
Pyrophosphate arthropathy is the term used for a chronic structural arthropathy related to CPP deposition.2,5
CPP crystal deposition disease
| ||||||||||||||||||||
- The epidemiology of CPPD crystal deposition is described in Table 2.6
- Most linked with advancing age (average age of 72).
TABLE 2 Epidemiology of Calcium Pyrophosphate Dihydrate Crystal Deposition
| Age Association | Rises With Age | ||
|---|---|---|---|
| Sex distribution | (F:M) 1:1 | ||
| Chondrocalcinosis prevalence | 8.1% (age range 63-93) | ||
| Pyrophosphate arthropathy prevalence | 3.4% (age range 40-89) | ||
| Geography | Appears ubiquitous | ||
| Genetic associations | Mutations of ANKH gene on chromosome 5p (CCAL2) and unknown genes on chromosome 8q (CCAL1) |
From Hochberg MC et al: Rheumatology, ed 5, St Louis, 2011, Mosby.
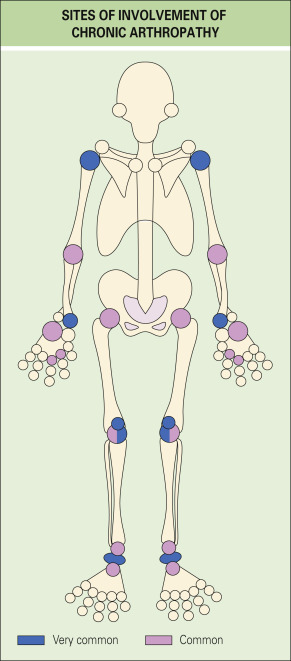
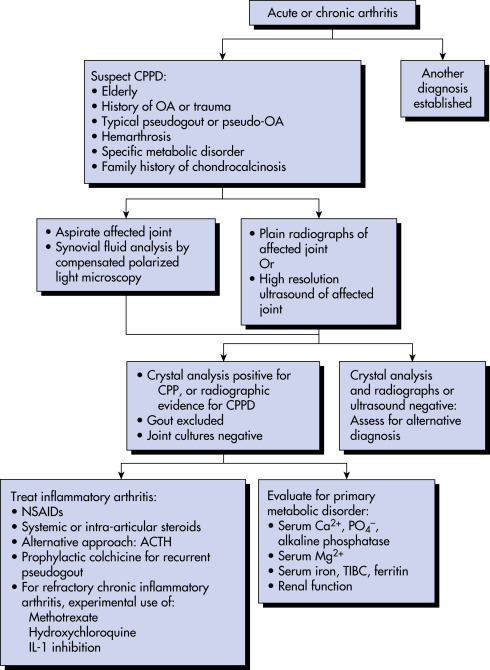
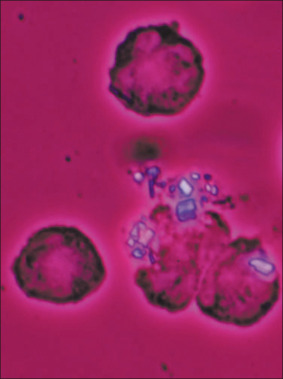
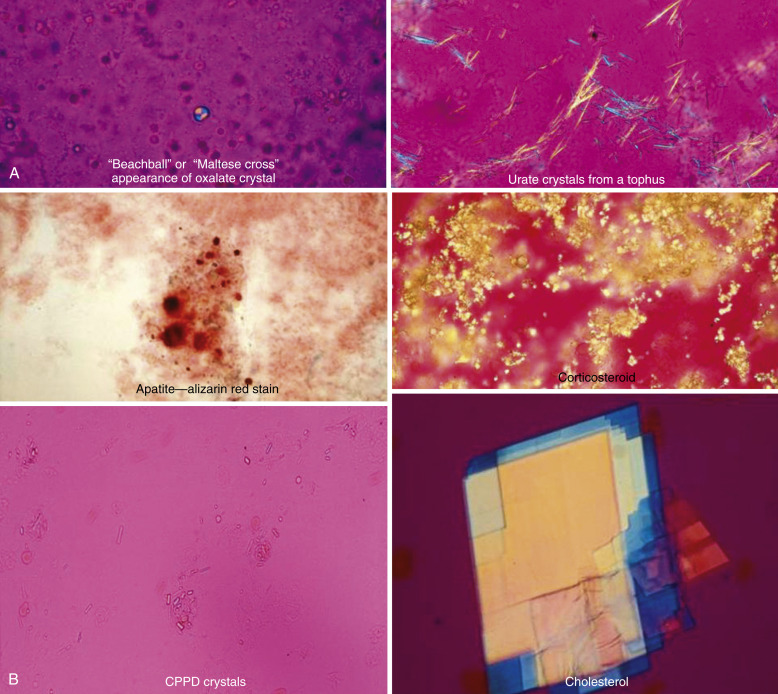
- Acute CPP crystal arthritis/pseudogout: Monoarticular attacks most commonly involve the knee and wrist but can be polyarticular (Fig. E1). Patients, especially the elderly, can have systemic manifestations such as fever and altered mental status and therefore diagnostic aspiration is essential to rule out septic arthritis. Situations that may trigger acute CPPD crystal arthritis are described in Box E1.6
- Asymptomatic disease (“asymptomatic CPPD”)
- Pseudogout (acute CPP crystal arthritis)
- Pseudo-RA (chronic CPP crystal inflammatory arthritis): Symmetric polyarthritis
- Pseudo-OA, with or without superimposed acute attacks (OA with CPPD)
- Pseudo-neuropathic joint disease
- Crowned-dens syndrome caused by crystal deposition in the ligamentum flavum of the cervical spine, either asymptomatic or causing acute neck pain
- Pseudo-polymyalgia rheumatica (pseudo-PMR): Pain and stiffness in the neck and shoulder girdle mimicking PMR
Cppd Often Involves Joints Not Typically Involved in Osteoarthritis.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
- Idiopathic
- Familial
- Trauma
- Metabolic and endocrine disorders (Table 3): Hyperparathyroidism, hypophosphatasia, hemochromatosis, hypomagnesemia, Gitelman syndrome, Bartter syndrome, gout, ochronosis, acromegaly, Wilson disease, familial hypocalciuric hypercalcemia, X-linked hypophosphatemic rickets.5,7
TABLE 3 Diseases Associated With Calcium Pyrophosphate Dihydrate Crystal Deposition Disease
| Disease | Strength of Evidence for a Link With CPPD | Recommended Testing |
|---|---|---|
| Hyperparathyroidism | Strong | Calcium, parathyroid hormone level |
| Hemochromatosis | Strong | Fe, TIBC, ferritin, C282Y |
| Hypophosphatasia | Strong | Alkaline phosphatase |
| Hypomagnesemia | Strong | Magnesium |
| Gout | Strong | Synovianalysis |
| Rheumatoid arthritis | Moderate | Clinical judgment |
| Osteoporosis | Moderate | Bone density if warranted |
CPPD, Calcium pyrophosphate dihydrate crystal deposition disease; TIBC, total iron-binding capacity.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.