AUTHOR: Daniel K. Asiedu, MD, PhD, FACP




DefinitionAlcoholic hepatitis (AH) is a severe, progressive, inflammatory, and cholestatic liver disease occurring in patients with long-term heavy alcohol use (60 to 80 g/day in men and 20 to 40 g/day in women). Main characteristics include rapid onset of jaundice, hepatomegaly, generalized malaise, and subtle systemic inflammatory response features.
SynonymAH
| ICD-10CM CODES | | K70.10 | Alcoholic hepatitis without ascites | | K70.9 | Alcoholic liver disease, unspecified |
|
Epidemiology & Demographics
- Approximately 2 million people in the U.S. (about 1% of the population) are affected by alcoholic liver disease.
- Alcoholic hepatitis accounts for 0.08% to 0.09% of admissions in the U.S.
- Typical presentation age: 40 to 50 yr. Majority occurs before age 60.
- Patients with alcoholic hepatitis typically drink more than 100 g of alcohol daily for two or more decades.
- Excessive alcohol intake is the third leading preventable cause of death in the U.S.
PrevalenceApproximately 25% to 30%
Predominant Sex & AgeThe majority of patients are males. Males are two times as likely as women to abuse alcohol. However, women develop alcoholic hepatitis after a shorter time and smaller amount of alcoholic exposure than men.
Risk FactorsDrinking multiple alcohol types, drinking alcohol between meal times, poor nutrition, female gender, obesity, Hispanic ethnicity, long-term ingestion of >10 to 20 g/day of alcohol in women and >20 to 40 g/day in men
GeneticsNo genetic predilection for any one race. In the U.S., however, there is increased incidence in minority groups.
Physical Findings & Clinical PresentationCommon presenting symptoms include:
- Rapid onset of jaundice within 60 days of heavy alcohol consumption (>50 g/day) for at least 6 mo
- Jaundice with duration <3 mo
- Right upper quadrant abdominal/epigastric pain
- Nausea/vomiting
- Malaise
- Low-grade fever
- Anorexia
- Abdominal distention/pain (due to ascites)
- Weight loss or malnourishment
- Proximal muscle wasting and weakness
- Complications of liver impairment (GI bleed; confusion, lethargy, ascites)
Findings on physical examination include:
- Jaundice and ascites
- Hepatomegaly, with tender liver on palpation
- Fever (first exclude other causes of fever, such as spontaneous bacterial peritonitis, urinary tract infection [UTI], pneumonia)
- Asterixis (a flapping tremor)
- Splenomegaly
- Tachycardia/tachypnea
- Hypotension
- Peripheral edema
- Abdominal distention with shifting dullness (ascites)
- Hepatic bruit (may occur in >50% of patients)
- With coexistent cirrhosis, look for:
- Gynecomastia
- Proximal muscles wasting
- Spider angiomata
- Altered hair distribution

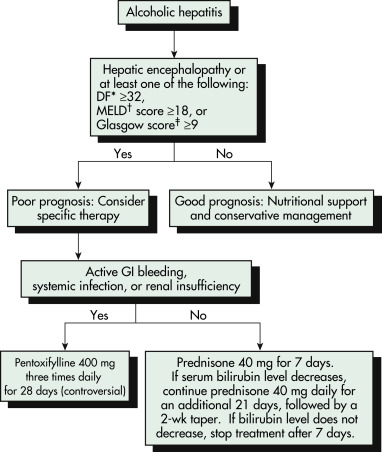
An algorithm for the management of patients with alcoholic hepatitis is described in Fig. E1. Treatment can be divided into three main components:
- Determining the severity of the disease using Maddrey Discriminant Function (DF) and Model for End Stage Liver Disease (MELD)
- Supportive care which includes lifestyle modifications and nutritional support
- Pharmacologic therapy
Figure E1 Algorithm for the Management of Patients with Alcoholic HepatitisThe DF is Calculated as Follows: 4.6 (Prothrombin Time of Patient – Prothrombin Time of Control) + Serum Bilirubin Level (in mg/dl). †the Model for End-Stage Liver Disease (MELD) Score is Based on the Serum Bilirubin Level, INR, and Serum Creatinine Level. ‡the Glasgow Alcoholic Hepatitis Score is Based on the Patient’s Age, White Blood Cell Count, Blood Urea Nitrogen Level, Ratio of Prothrombin Time to a Control Value, and Serum Bilirubin Level. DF, Discriminant Function; GI, Gastrointestinal. Online Calculators for These Various Models are Available at www.lillemodel.com.

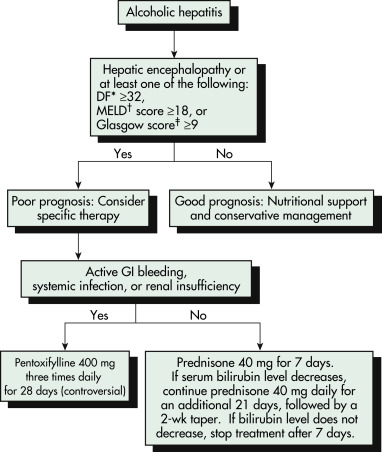
Modified from Feldman M et al: Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.
Lifestyle Modifications
- Abstinence, together with adequate nutritional support, is the cornerstone of management.
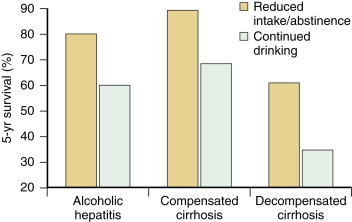
- Abstinence from alcohol (this improves both short- and long-term survival). Fig. E2 describes the effect of subsequent alcohol intake on 5-yr survival in patients with alcoholic hepatitis.
- Nonpharmacologic methods to promote abstinence include cognitive-behavioral therapy (CBT), Alcoholics Anonymous (AA) attendance, and motivational interviewing.
- Pharmacologic aids include using naltrexone, acamprosate, or baclofen.
- Monitor abstinence with breath test or urine drug screen (for use in past 3 days) or hair sample analysis for ethyl glucuronide (test alcohol intake within the last few months).
- Smoking cessation (to decrease oxidative stress).
- Treatment of substance abuse.
Figure E2 Effect of Subsequent Alcohol Intake on 5-Yr Survival in Patients with Alcoholic Hepatitis and Cirrhosis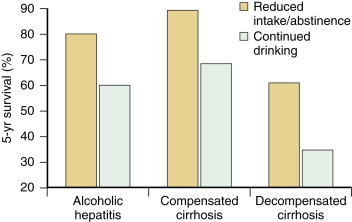
From Day CP: Liver disorder part 1 of 2, Medicine 35(1):22-25, 2007.
Nutritional Support:
- Good nutrition is an essential part of treatment because many patients with alcoholic hepatitis have severe protein-calorie malnutrition as well as deficiencies of trace minerals and several vitamins.
- Nutritional support includes:
- Liberal vitamin supplementation (especially thiamine, folic acid, vitamin K)
- Mineral supplementation (but not iron)
- Calorie counting is essential. A high calorie intake (1.2 to 1.4 times the normal resting intake) may be required
- Protein intake of 1.2 to 1.5 g/kg of ideal body weight per day will provide adequate support. Exception: In patients with severe encephalopathy, protein restriction may be required.
- Fluid management
Pharmacologic TherapySevere alcoholic hepatitis may require treatment. Severity can be assessed by calculating the MELD score or MDF score or the Glasgow score.
- An MDF score ≥32 indicates significant or severe alcoholic hepatitis (30-day mortality of 50%).
- MELD score can easily be calculated (visit https://optn.transplant.hrsa.gov/resources/allocation-calculators/meld-calculator/). This score predicts short-term survival in patients with cirrhosis. A score >20 predicts increased short-term mortality.
- Glasgow score: Contains four variables (BUN, PT, WBC count, and bilirubin). A score ≥9 indicates increased mortality.
Indications for hospitalization include:
- MDF ≥32
- MELD >20
- Glasgow score >8
- Hepatic encephalopathy
Patients with severe alcoholic hepatitis may be treated with glucocorticosteroids (prednisolone 40 mg/day for 28 days with a 2-wk taper). Glucocorticosteroids reduce hepatic injury, suppress inflammation, and promote liver regeneration. However, not all studies have demonstrated consistent therapeutic benefits for steroids, even in high-risk patients.1 Prednisolone should be discontinued if bilirubin does not decrease by day 17. An alternative agent for patients with contraindications to corticosteroids is pentoxifylline. Pentoxifylline is not effective in patients who do not respond to prednisone, and data supporting its use is weak.
Liver Transplantation
- Liver transplantation could be considered for patients with MELD >26 and unresponsive to steroids.
- Usually reserved for patients with end-stage liver disease. Patients whose hepatitis is not responding to medical therapy have a 6-mo survival rate of approximately 30%. Since most hepatitis deaths occur within 2 mo, early liver transplantation is attractive and associated with higher than 80% survival at 3 yr.
- Patients with alcoholic hepatitis must be sober for at least 6 mo before they can be eligible for consideration for liver transplantation. However, transplantation candidates should not be based solely on 6 mo abstinence, and other factors, such as social support and need for rehabilitation, should be considered.
ReferralSevere acute alcoholic hepatitis may require intensive care unit (ICU) care and referral to different subspecialists:
- GI/hepatology (for patients with evidence of GI hemorrhage)
- Nutritional services
- Nephrology (for acute renal failure, hepatorenal syndrome)
- Neurology (for change in mental status, seizures)
- Infectious disease (for fever/leukocytosis)