AUTHOR: Fred F. Ferri, MD
- Cushing syndrome is the occurrence of clinical abnormalities associated with glucocorticoid excess as a result of exaggerated adrenal cortisol production or long-term glucocorticoid therapy.
- Cushing disease is Cushing syndrome caused by pituitary adrenocorticotropic hormone (ACTH) excess.
| ||||||||||||||||||||||||||||
- Hypertension.
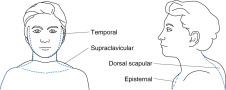
- Central obesity with rounding of the facies (moon facies); thin extremities. Fig. 1 illustrates the distribution of adipose tissue in Cushing syndrome.
- Hirsutism, menstrual irregularities, hypogonadism.
- Skin fragility, ecchymoses, red-purple abdominal striae (Fig. E2), acne, poor wound. healing, hair loss, facial plethora, hyperpigmentation (with ACTH excess). The frequency of individual findings in Cushing syndrome is summarized in Table 1.
- Psychosis, emotional lability, paranoia.
- Muscle wasting with proximal myopathy.
TABLE 1 Cushing Syndrome-Frequency of Individual Findings
| Physical Finding∗ | Frequency (%)† | ||
|---|---|---|---|
| Vital Signs | |||
| Hypertension | 64-88 | ||
| Body Habitus | |||
| Moon facies | 67-92 | ||
| Central obesity | 44-97 | ||
| Buffalo hump | 34-75 | ||
| Skin Findings | |||
| Thin skin | 27 | ||
| Plethora | 28-94 | ||
| Hirsutism, women | 48-81 | ||
| Ecchymoses | 23-75 | ||
| Red or purple striae | 46-68 | ||
| Acne | 21-52 | ||
| Extremity Findings | |||
| Proximal muscle weakness | 39-68 | ||
| Edema | 15-66 | ||
| Other | |||
| Significant depression | 12-40 | ||
∗Diagnostic standard: For Cushing syndrome, elevated daily cortisol or corticosteroid metabolites, or both, with loss of circadian rhythm and with abnormal dexamethasone suppression tests.
† Results are overall mean frequency or, if statistically heterogeneous, the range of values.
From McGee S: Evidence-based physical diagnosis, ed 4, Philadelphia, 2018, Elsevier.
Figure 1 Distribution of adipose tissue in Cushing syndrome.
Rounding of the cheeks and prominent bitemporal fat produce the characteristic moon facies. Fat also may accumulate bilaterally above the clavicles (supraclavicular collar), in front of the sternum (episternal area, or dewlap), and over the back of the neck (dorsal cervical fat pad, or buffalo hump). In these drawings, the dotted line depicts normal contours of patients without Cushing syndrome.
From McGee S: Evidence-based physical diagnosis, ed 4, Philadelphia, 2018, Elsevier.
Note that the previously described characteristics are not commonly present in Cushing syndrome caused by ectopic ACTH production. Many of these tumors secrete a biologically inactive ACTH that does not activate adrenal steroid synthesis. These patients may have only weight loss and weakness.
Figure E2 Clinical features of Cushing syndrome.
A, Centripetal and some generalized obesity and dorsal kyphosis in a 30-yr-old woman with Cushing disease. B, Same patient as in A showing moon facies, plethora, hirsutism, and enlarged supraclavicular fat pads. C, Facial rounding, hirsutism, and acne in a 14-yr-old girl with Cushing disease. D, Central and generalized obesity and moon facies in a 14-yr-old boy with Cushing disease. E and F, Typical centripetal obesity with livid abdominal striae seen in a 41-yr-old woman (E) and a 40-yr-old man (F) with Cushing syndrome. G, Striae in a 24-yr-old patient with congenital adrenal hyperplasia treated with excessive doses of dexamethasone as replacement therapy. H, Typical bruising and thin skin of a patient with Cushing syndrome. In this case, the bruising occurred without obvious injury.
From Melmed S et al: Williams textbook of endocrinology, ed 12, Philadelphia, 2011, Saunders.
- Iatrogenic from long-term glucocorticoid therapy (common)
- Pituitary ACTH excess (Cushing disease; 60%)
- Adrenal neoplasms (30%)
- Ectopic ACTH production (neoplasms of lung, pancreas, kidney, thyroid, thymus; 10%)
- Table 2 summarizes the incidence of tumors associated with the ectopic ACTH syndrome
- A classification of causes of Cushing syndrome is described in Table 3
TABLE 3 Classification of Causes of Cushing Syndrome
| ACTH-Dependent Causes | |||
| Cushing disease (pituitary-dependent) | |||
| Ectopic ACTH syndrome | |||
| Ectopic CRH syndrome | |||
| Macronodular adrenal hyperplasia | |||
| Iatrogenic (treatment with 1-24 ACTH) | |||
| ACTH-Independent Causes | |||
| Adrenal adenoma and carcinoma | |||
| Primary pigmented nodular adrenal hyperplasia and Carney syndrome | |||
| McCune-Albright syndrome | |||
| Aberrant receptor expression (gastric inhibitory polypeptide, interleukin-1β) | |||
| Iatrogenic (e.g., pharmacologic doses of prednisolone, dexamethasone) | |||
| Pseudo-Cushing Syndromes | |||
| Alcoholism | |||
| Depression | |||
| Obesity |
ACTH, Adrenocorticotropic hormone; CRH, corticotropin-releasing hormone.
From Melmed S et al: Williams textbook of endocrinology, ed 12, Philadelphia, 2011, Saunders.
TABLE 2 Tumors Associated With the Ectopic Adrenocorticotropic Hormone Syndrome
| Tumor Type | Approximate Incidence (%) | ||
|---|---|---|---|
| Small cell lung carcinoma | 50 | ||
| Non-small cell lung carcinoma | 5 | ||
| Pancreatic tumors (including carcinoids) | 10 | ||
| Thymic tumors (including carcinoids) | 5 | ||
| Lung carcinoids | 10 | ||
| Other carcinoids | 2 | ||
| Medullary carcinoma of thyroid | 5 | ||
| Pheochromocytoma and related tumors | 3 | ||
| Rare carcinomas of prostate, breast, ovary, gallbladder, colon | 10 |
From Melmed S et al: Williams textbook of endocrinology, ed 12, Philadelphia, 2011, Saunders.