AUTHORS: Helen B. Gomez Slagle, MD and Anthony Sciscione, DO
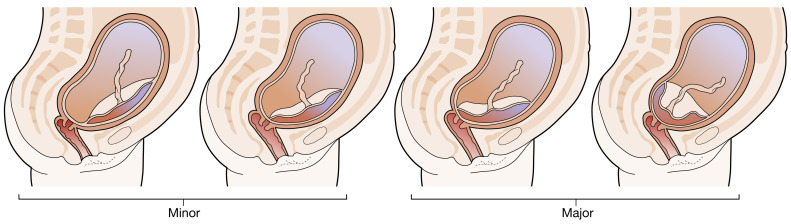
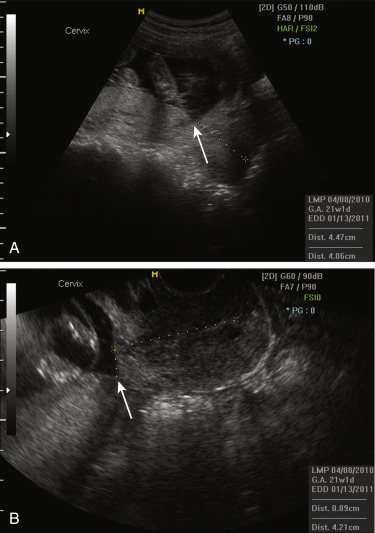
The diagnosis of placenta previa is based on sonography and requires the identification of echogenic homogeneous placental tissue over the internal cervical os. When the placental edge is <2 cm from the internal os, the placenta is called “low-lying.” The historic terms “marginal” and “partial” for characterizing a placenta previa are no longer used. A classification of placenta previa in “major” or “minor” is described in Table 1 and illustrated in Fig. 1.
TABLE 1 Classification of Placenta Previa
| Minor | I | Encroaches the lower uterine segment |
| II | Reaches internal os of the cervix (marginal) | |
| Major | III | Covers part of internal os (partial) |
| IV | Completely covers the internal os (complete) |
From Magowan BA: Clinical obstetrics and gynecology, ed 4, London, 2019, Elsevier.
In the presence of a cesarean section scar, an anterior placenta previa may result in abnormal invasion (morbidly adherent placenta, placenta accreta).
From Magowan BA: Clinical obstetrics and gynecology, ed 4, London, 2019, Elsevier.
One hypothesis is that the lower uterine cavity contains more vascularized decidua, which promotes implantation of trophoblast toward the cervical os. Another hypothesis is that a particularly large placental surface area increases the probability that the placenta will implant over the cervical os.
| ||||||||||||||||||||||||||||||||
The pooled prevalence of major placenta previa was 4.3 cases/1000 pregnancies. Prevalence was highest among Asian studies (12.2/1000) and lower among studies from Europe (3.6/1000), North America (2.9/1000), and sub-Saharan Africa (2.7/1000).
- Previous placenta previa (recurs in 4% to 8% of subsequent pregnancies)
- Previous cesarean delivery (increases incidence by 47% to 60%)
- Multiparity
- Multiple gestation (increases prevalence by 40%)
- Smoking and cocaine use
- Previous intrauterine surgical procedure or Asherman syndrome
- Abnormal or large placenta
The classic presentation of placenta previa is painless vaginal bleeding, usually in the second or third trimester. 10% to 20% of women present with uterine contractions, pain, and bleeding. On physical examination, the uterus is soft and pain free. The fetus is often in breech, transverse lie, or high. Fetal distress is usually not present.