AUTHORS: Nirav Haribhakti, MD, PharmD and John L. Reagan, MD

DefinitionThe HELLP syndrome is a serious variant of preeclampsia. HELLP is an acronym for hemolysis, elevated liver enzymes, and low platelet count. It is the most frequently encountered microangiopathy of pregnancy. Two classification systems exist (Mississippi Classification and Tennessee Classification); degree of maternal thrombocytopenia is a primary indicator of disease severity (Table E1).
SynonymsHELLP
Hemolysis
Elevated liver enzymes
Low platelet syndrome
| ICD-10CM CODES | | O14.2 | HELLP syndrome | | O26.892 | Other specified pregnancy related conditions, second trimester | | O26.893 | Other specified pregnancy related conditions, third trimester | | O26.899 | Other specified pregnancy related conditions, unspecified trimester | | O26.90 | Pregnancy related conditions, unspecified, unspecified trimester | | O26.91 | Pregnancy related conditions, unspecified, first trimester | | O26.92 | Pregnancy related conditions, unspecified, second trimester | | O26.93 | Pregnancy related conditions, unspecified, third trimester |
|
Table E1 Two Classification Systems for HELLP Syndrome
| Tennessee | Mississippi |
|---|
| Class 1: | Platelets <100,000/mm3 AST or ALT >70 IU/L | Platelets <50,000/mm3 AST or ALT >70 IU/L |
| Class 2: | | Platelets >50,000/mm3 to <100,000/mm3 AST or ALT >70 IU/L |
| Class 3: | | Platelets >100,000/mm3 to <150,000/mm3 AST or ALT ≥70 IU/L |
ALT, Alanine aminotransferase; AST, aspartate aminotransferase; HELLP, hemolysis, elevated liver enzymes, and low platelet count. All criteria require LDH ≥600 IU/L.
Epidemiology & Demographics
- HELLP is a rare complication occurring in <1% of total pregnancies, but the rate is estimated to be around 5% to 20% in pregnancies with severe preeclampsia.
- About 20% of patients may not have hypertension, and about 10% of patients may not have proteinuria.
- About 70% of the cases happen antepartum and 30% postpartum.
- Of the patients diagnosed with HELLP syndrome antepartum, 70% are diagnosed in the third trimester peaking between 27 and 37 wk of gestation.
- Younger age, headache, bilirubin >2.0, lactate dehydrogenase (LDH) >1290, and platelets <50,000 are predictive of worse maternal outcomes.
Risk Factors
- Patients with history of preterm preeclampsia or HELLP syndrome in a previous pregnancy are at increased risk of HELLP syndrome in subsequent pregnancies.
Recurrence Rate2% to 27%.
Physical Findings & Clinical Presentation
- Although many women with HELLP syndrome are asymptomatic, 40% to 80% report right upper quadrant or epigastric pain, 29% to 84% have nausea and vomiting, and 33% to 61% have headache.
EtiologyAs with other microangiopathies, endothelial dysfunction, with resultant activation of the intravascular coagulation cascade, has been proposed as the central pathogenesis of HELLP syndrome.

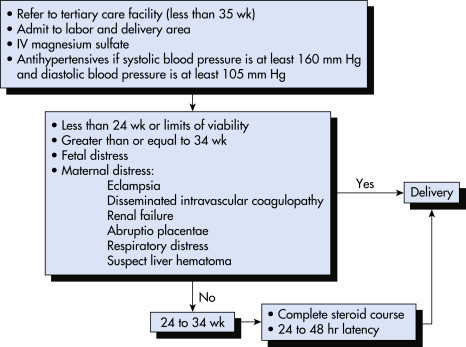
Treatment depends on gestational age of the fetus, severity of condition, and maternal status. Stabilization of the mother is the first priority. Fig. E1 describes an algorithm for the management of HELLP syndrome.
Figure E1 An algorithm for the management of HELLP syndrome.

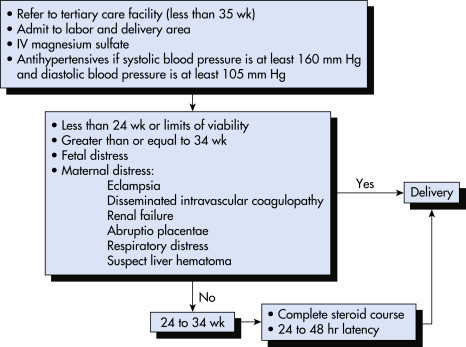
IV, Intravenous.
From Gabbe SG: Obstetrics, ed 6, Philadelphia, 2012, Saunders.
Acute General Rx
- Assess gestational age thoroughly. Fetal status should be monitored with nonstress tests, contraction stress tests, and/or biophysical profile.
- Maternal status should be evaluated by history, physical examination, and laboratory testing.
- Magnesium sulfate is administered for seizure prophylaxis regardless of blood pressure.
- Blood pressure control is achieved with agents such as hydralazine or labetalol.
- Indwelling Foley catheter to monitor maternal volume status and urine output.
- Eculizumab has also been proposed as a possible therapy in case reports.
Chronic Rx
- If the gestational age is greater than 34 wk or if nonviable fetus, consider delivery after maternal stabilization.
- If gestational age is between 27 to 34 wk, and there are no complications such as multiorgan dysfunction, disseminated intravascular coagulation, renal failure, placental abruption, or liver hemorrhage, consider administration of corticosteroid for fetal lung maturation and delivery within 48 h.
- Some reports have shown temporary amelioration of HELLP severity with the administration of high-dose steroids (e.g., dexamethasone 10 mg q12h) measured by increased urine output, improvement in platelet count, and liver function test. A 2015 meta-analysis of multiple studies suggested improvement in lab parameters and decreased length of intensive care unit stay with steroid administration. However, there was not better maternal mortality and morbidity.
- Judicious use of blood products, especially in those requiring surgery.
- The patient requires intensive observation. Laboratory levels may worsen immediately postpartum but should begin to improve within 48 h.
- Hepatic hematoma and its rupture is a potentially fatal complication that warrants promptly consulting a surgical team experienced in liver trauma surgery.
DispositionThe natural history of this disorder is a rapidly deteriorating condition requiring close monitoring of maternal and fetal well-being.
ReferralPreterm patients with HELLP syndrome should be stabilized hemodynamically and transferred to a tertiary care center. Term patients can be treated at a local hospital depending on the availability of obstetric, neonatal, and blood banking services.