AUTHOR: Lynn C. Fullenkamp, MD, JD
Otitis externa refers to a variety of conditions causing inflammation and/or infection of the external auditory canal (and/or auricle and tympanic membrane).1 There are six subgroups of otitis externa:
| ||||||||||||||||||||||||
- Diffuse otitis externa is most often seen in swimmers and in hot, humid climates, conditions that lead to water retention in the ear canal. In the U.S., 44% of AOE-related healthcare visits occur June to August1
- Necrotizing otitis externa is more common in elderly, diabetics, and immunocompromised patients3
The two most common symptoms are otalgia, ranging from pruritus to severe pain exacerbated by motion (e.g., chewing), and otorrhea. Patients may also experience aural fullness and hearing loss due to swelling and occlusion of the canal. More intense symptoms may occur with bacterial otitis externa, with or without fever, and lymphadenopathy (anterior to tragus).1 Findings unique to specific forms of the infection include:
- Acute localized otitis externa (furunculosis)1:
- Impetigo1:
- Erysipelas1:
- Eczematous or seborrheic otitis externa1:
- Stems from a variety of dermatologic problems that can involve the external auditory canal
- Severe itching, erythema, scaling, crusting (Fig.E1), and fissuring possible
From Cherry JD et al: Feigin and Cherry’s pediatric infectious diseases, ed 8, Philadelphia, 2019, Elsevier.
- Acute diffuse otitis externa (swimmer ear)1:
- Begins with itching and a feeling of pressure and fullness in the ear that becomes increasingly tender and painful
- Mild erythema and edema of the external auditory canal, which may cause narrowing and occlusion of the canal (Fig. E2), leading to hearing loss
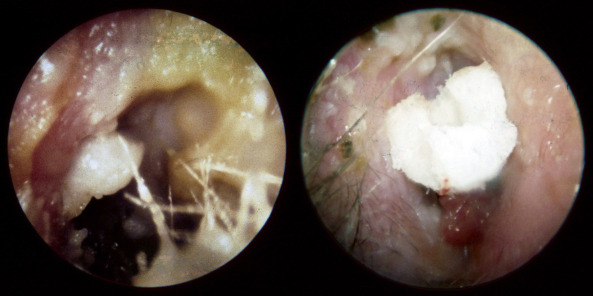
Figure E2 Acute otitis externa.
Erythema, edema, and copious purulent debris are seen in the left image, and in some cases, an edematous canal with granulation tissue (right) necessitates the placement of an ear wick to facilitate topical drug delivery in the acute setting.
Courtesy John House, MD. In Flint PW et al: Cummings otolaryngology, head and neck surgery, ed 7, Philadelphia, 2021, Elsevier.
- Otomycosis1:
- Chronic otitis externa1:
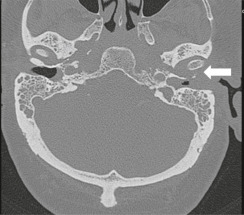
- Necrotizing otitis externa (also known as malignant otitis externa). Typically seen in older patients with diabetes or in patients who are immunocompromised3
- Redness, swelling, and tenderness of the ear canal
- Classic finding of granulation tissue on the floor of the canal and the bone-cartilage junction
- Small ulceration of necrotic soft tissue at bone-cartilage junction
- Most common symptoms: Pain (often severe) and otorrhea
- Lessening of purulent drainage as infection advances
- As the infection advances, osteomyelitis of the base of the skull and temporomandibular joint osteomyelitis can develop
- Facial nerve palsy often the first and only cranial nerve defect
- Possible involvement of other cranial nerves
- Box 1 summarizes common pathogens in otitis externa
- Acute localized otitis externa: Staphylococcus aureus
- Impetigo:
- Erysipelas: GAS
- Eczematous otitis externa:
- Acute diffuse otitis externa:
- Otomycosis:
- Chronic otitis externa: Persistent low-grade infection and inflammation
- Necrotizing otitis externa (NOE)3:
- Complication of persistent otitis externa
- Typically starts in the external auditory canal and spreads to the stylomastoid foramen, then to the mastoid tip and the jugular foramen. Finally, it extends to the petrous apex and the middle cranial fossa
- P. aeruginosa
- High index of suspicion for atypical organisms (MRSA) in patients without diabetes