AUTHOR: Vanita B.D. Jain, MD
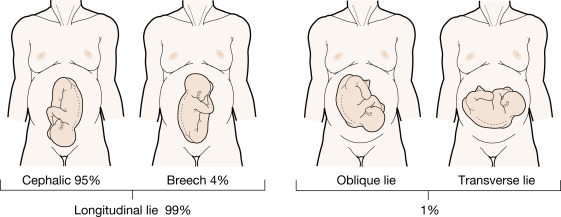
Near term or during labor, the fetus normally assumes a vertical orientation (lie) and cephalic presentation.1 Breech presentation occurs when fetal longitudinal axis is such that the cephalic pole occupies the uterine fundus (Fig. E1). Three types exist: Frank (flexed hips, extended knees or pike position), complete (flexed hips and knees tuck position), and footling (hips extended).1
| ||||||||||||||||||||||||||||||||
Mixed data with Term Breech Trial (2000) showed increased perinatal mortality, neonatal mortality, and neonatal morbidity based on mode of delivery.3 However, more recently published data contradicts these original findings as long as specific hospital protocol guidelines (for both eligibility and labor management) are followed.3
- Diagnosis can be made by abdominal palpation, vaginal examination, or ultrasound1
- Lack of presenting part on vaginal examination
- Fetal heart tones heard above the umbilicus
- Leopold maneuvers revealing mobile fetal part in the uterine fundus