AUTHOR: Fred F. Ferri, MD
Rosacea is a common, chronic, heterogenous, inflammatory skin disease, seen most often in adults of both genders and all skin types. It predominantly involves the central face and is characterized by intermittent flares that present with transient findings (flushing, papules/pustules) and by persistence of some fixed clinical manifestations (telangiectasias, persistent facial erythema).
| ||||||||||||||||||||||||
- Facial erythema, presence of papules, pustules, and telangiectasia (Fig. E1).
- Excessive facial warmth and redness are the predominant presenting symptoms.
- Itching is generally absent.
- Comedones are absent (unlike acne).
- Women are more likely to show symptoms on the chin and cheeks, whereas in men the nose is commonly involved.
- Ocular findings (mild dryness and irritation with blepharitis, conjunctival injection, burning, stinging, tearing, eyelid inflammation, swelling, and redness) are present in 50% of patients.
Rosacea can be classified into four major subtypes (Table E1):
- Erythematotelangiectatic (vascular): Erythema in central part of face, telangiectasia, flushing
- Papulopustular (inflammatory): Presence of dome-shaped erythematous papules and small pustules, in addition to facial erythema, flushing, and telangiectasia
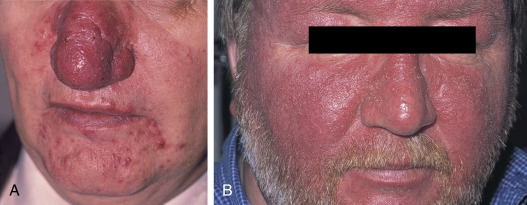
- Phymatosis/glandular rosacea (Fig. E2): Presence of thickened skin with prominent pores that may affect the nose (rhinophyma) (Fig. E3), chin (gnathophyma), forehead (metophyma), eyelids (blepharophyma), and ears (otophyma)
- Ocular: Conjunctival injection, sensation of foreign body in the eye, telangiectasia and erythema of lid margins, scaling
Figure E1 Papulopustular rosacea.
Courtesy Curt Samlaska, MD. From James WD et al: Andrews’ diseases of the skin, ed 12, Philadelphia, 2016, Elsevier.
A, Note the Scattered Papules on the Face and the Confluent Involvement of the Nose. Alcohol Ingestion is Not Related to This Appearance. B, Note the Severe Inflammation with Confluent Redness and Significant Edema.
From White GM, Cox NH [eds]: Diseases of the skin: a color atlas and text, ed 2, St Louis, 2006, Mosby.
TABLE E1 Differential Diagnosis of the Four Subtypes of Rosacea∗
| Rosacea Subtype and Differential Diagnosis | Distinguishing Feature(s) From Rosacea | ||
|---|---|---|---|
| Erythematotelangiectatic rosacea | |||
| Actinic damage (telangiectatic photoaging) | |||
| Seborrheic dermatitis | |||
| Keratosis pilaris rubra | |||
| Acute cutaneous lupus erythematosus | |||
| Flushing (idiopathic or secondary) |
| ||
| Papulopustular rosacea | |||
| Acne (vulgaris) | |||
| Steroid-induced rosacea | |||
| Demodicosis (Demodex folliculitis) |
| ||
| Pityriasis folliculorum | |||
| Tinea incognito, candidiasis | |||
| Papulopustular eruptions due to EGFR inhibitors | |||
| Follicular mucinosis | |||
| Ocular rosacea | |||
| Seborrheic dermatitis | |||
| Drug-induced ocular rosacea | |||
| Phymatous rosacea | |||
| Lupus pernio (sarcoidosis) | |||
| Discoid lupus erythematosus | |||
| Lupus vulgaris (cutaneous TB) | |||
| Neoplasms | |||
EGFR, Epidermal growth factor receptor; KOH, potassium hydroxide; SLE, systemic lupus erythematosus; TB, tuberculosis.
∗Occasionally, trichostasis spinulosa has associated erythema, but detection of multiple hairs within the follicular orifice by dermoscopy or microscopic examination of follicular contents establishes the diagnosis.
From Bolognia JL: Dermatology, ed 4, Philadelphia, 2018, Elsevier.
- The pathophysiology of rosacea is incompletely understood but believed to involve the vasculature.
- Hot drinks, alcohol, and sun exposure may accentuate the erythema by causing vasodilation of the skin.
- Flare-ups may also result from reactions to medications (e.g., simvastatin, ACE inhibitors, vasodilators, fluorinated corticosteroids), stress, extreme heat or cold, wind, humidity, strenuous exercise, spicy drinks, menstruation.