AUTHOR: Kelly Ruhstaller, MD
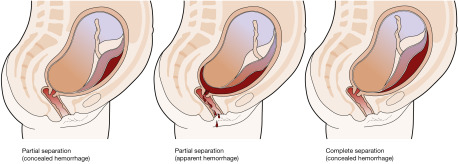
Abruptio placentae is the separation of placenta from the uterine wall before delivery of the fetus. The condition occurs in approximately 1% of pregnancies. There are three classes of abruption (Fig. 1) based on maternal and fetal status, including an assessment of uterine contractions, quantity of bleeding, fetal heart rate monitoring, and abnormal coagulation studies (fibrinogen, prothrombin time, partial thromboplastin time).
- Grade I: Mild vaginal bleeding, uterine irritability, stable vital signs, reassuring fetal heart rate, normal coagulation profile (fibrinogen 450 mg/dl). Approximately half of abruptions are grade I.
- Grade II: Moderate vaginal bleeding, hypertonic uterine contractions, orthostatic blood pressure measurements, unfavorable fetal status, fibrinogen 150 to 250 mg. Approximately a quarter of abruptions are grade II.
- Grade III: Severe bleeding (may be concealed), hypertonic uterine contractions, overt signs of hypovolemic shock, fetal death, thrombocytopenia, fibrinogen <150 mg/dl. Approximately a quarter of abruptions are grade III.
Premature separation of placenta
| ||||||||||||||||||||||||||||||||
5% to 17%, some studies showing a 5- to 10-fold increase in risk; with two prior episodes, 25%.
Hypertension (greatest association), trauma, polyhydramnios, multifetal gestation, smoking, use of cocaine, chorioamnionitis, preterm premature rupture of membranes. Table 1 summarizes placental abruption risk factors.
- Triad of uterine bleeding (concealed or per vagina), hypertonic uterine contractions or signs of preterm labor, and evidence of fetal compromise exists.
- More than 80% of cases have external bleeding; 20% of cases have no bleeding but have indirect evidence of abruption, such as failed tocolysis for preterm labor.
- Tetanic uterine contractions are found in only 17%.