AUTHOR: Glenn G. Fort, MD, MPH


DefinitionChronic rhinosinusitis (CRS) is an inflammatory condition that involves the paranasal passages and linings of the nasal passages that lasts 12 wk or longer despite medical therapy. It can be divided into three categories:
- CRS without nasal polyposis
- CRS with nasal polyposis
- Allergic fungal rhinosinusitis
SynonymsChronic sinusitis
CRS
| ICD-10CM CODE | | J32 | Chronic sinusitis, unspecified |
|
Epidemiology & DemographicsIncidenceCRS occurs in children and adults but is most frequently diagnosed in young and middle-aged adults.
PrevalenceIn the U.S. it varies from 1% to 5%.
Predominant Sex & AgeSome studies suggest women are more affected. In adults, the mean age of diagnosis was 39 yr.
Risk Factors
- Environmental or behavioral risk factors include:
- Smoking
- Cocaine use
- Chemical and air pollutants: Ozone, sulfur dioxide, nitrogen dioxide
- Host-associated risk factors: Allergic rhinitis, atopy, asthma, aspirin-exacerbated respiratory disease
- Innate immunodeficiencies: Cystic fibrosis
- Humoral immunodeficiencies: Common variable immunodeficiency, immunoglobulin A (IgA) or IgG subclass deficiencies, types of vasculitis (e.g., Churg-Strauss syndrome), and sarcoidosis
- Allergic fungal sinusitis
- Gastroesophageal reflux disease
- Odontogenic: Infectious agents from maxillary posterior teeth may breech into maxillary sinus
GeneticsPatients with cystic fibrosis or primary ciliary dyskinesia are more likely to develop CRS.
Physical Findings & Clinical Presentation
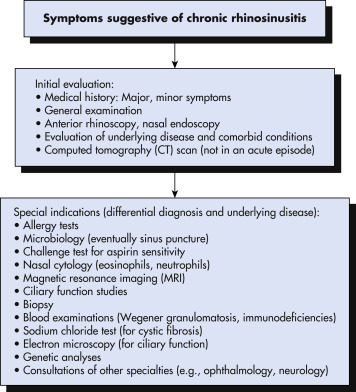
- CRS is diagnosed clinically with a physical examination and a detailed sinonasal history. There should be at least two out of the four cardinal symptoms for at least 12 consecutive wk:
- Nasal obstruction: 81% to 95% of patients
- Nasal drainage: 51% to 83% of patients
- Facial pain/pressure: 70% to 85% of patients
- Hyposmia/anosmia: 61% to 69% of patients
- Objective evidence on physical examination using anterior rhinoscopy and nasal endoscopy includes mucopurulent drainage, edema, polyps in the middle meatus
- Radiographic evidence includes, preferably, computed tomography (CT) of sinuses.
- Features of specific subtypes:
- CRS without nasal polyposis: Most common type (60% to 65% of cases) with cardinal clinical symptoms
- CRS with nasal polyposis: Characterized with the presence of bilateral nasal polyps in the middle meatus, which are translucent masses composed of gelatinous inflammatory material, as well as cardinal clinical symptoms
- Allergic fungal rhinosinusitis:
- Type 1 hypersensitivity confirmed by history, skin test, or serology
- Nasal polyposis
- Positive fungal stain
- Eosinophilic mucin showing fungal hyphae without tissue invasion
- CT of sinuses showing high-attenuation sinus contents with bony remodeling
Etiology
- Not fully understood but multifactorial involving host genetics and immunity, as well as environmental and infectious agents that produce chronic inflammation of the upper airways.
- Various cells, including fibroblasts, epithelial cells, endothelial cells, mast cells, eosinophils, antigen-presenting cells (dendritic cells), T cells, and B cells, have been shown to coordinate the immune inflammatory network underlying CRS, by the production of mediators such as cytokines, chemokines, eicosanoids, and antibodies.
- Microbiology: Organisms that may be involved in the pathogenesis of CRS include:
- Staphylococcus aureus: This is the most common bacterium and contributes to polyp formation. Methicillin-resistant S. aureus is isolated in 2% to 20% of patients with CRS.
- Coagulase-negative staphylococci: It is not always clear whether they are pathogens or colonizers.
- Pseudomonas aeruginosa: Occurs especially in patients with cystic fibrosis. Other gram-negative rods include Klebsiella pneumoniae, Proteus mirabilis, Enterobacter spp., and E. coli.
- Anaerobic bacteria include Peptostreptococcus, Fusobacterium, Prevotella spp., Porphyromonas spp.

The goal of treatment is to manage symptoms and to improve or maintain quality of life. Therapies are targeted to enhancing mucociliary clearance, improving sinus drainage/outflow, eliminating local infection and inflammation, and improving access for topical medications.
Nonpharmacologic TherapyNasal saline irrigation: Low-pressure, high-volume (240 mL) isotonic or hypertonic saline irrigation can reduce symptoms in 50% of patients and is better than nasal saline spray. Often used in conjunction with intranasal corticosteroid spray.
Acute General Rx
- Topical intranasal corticosteroids: First-generation products include beclomethasone dipropionate (QNASL), flunisolide (Nasalide, Nasarel), budesonide (Rhinocort), and triamcinolone acetonide (Nasacort). Newer agents include fluticasone propionate (Flonase), fluticasone furoate (Veramyst), mometasone furoate (Asmanex), and ciclesonide (Omnaris). Most are used once a day.
- Oral corticosteroids: Oral corticosteroids, such as prednisone, can be used in patients with severe disease and especially in patients with nasal polyps because they will help reduce the size of polyps. Prednisone will also minimize mucosal inflammation in allergic fungal rhinosinusitis. Dose: 20 mg twice daily for 5 days, then 20 mg daily for 5 days.
- Antibiotics: Often used in conjunction with prednisone. Can be used when evidence of infection present: Facial pain, air-fluid level on sinus CT, or purulent mucus in middle meatus. Use for up to 3 to 4 wk at most. Examples include amoxicillin/clavulanic acid or moxifloxacin.
SurgeryEndoscopic surgery is appropriate if medical therapy fails. It can provide ventilation and drainage of the paranasal sinuses and enlarge the paranasal sinuses to create better access for topical medications. In general, it does not cure the condition, and patients will need continued medical therapies.
Chronic RxUse of macrolide antibiotics for prolonged periods has been tried, but studies have not shown additional benefit.
Complementary & Alternative MedicineHerbal medicines, homeopathy, acupuncture, reflexology, and yoga are used but have not been studied in clinical trials.
Referral
- Otolaryngologist for long-term treatments and possible surgery