AUTHOR: Corey Elam Goldsmith, MD, FAAN
- Optic atrophy is identified weeks to months after an initial insult such as optic neuritis, trauma, or ischemia. May occur insidiously with no acute inciting event in more genetic or toxic causes. Frequently, it is noted by the physician during a routine eye exam.
- Asymmetry of disc color is often first subtle finding.
- Temporal part of optic disc is pale initially; later, the entire disc becomes pale/white.
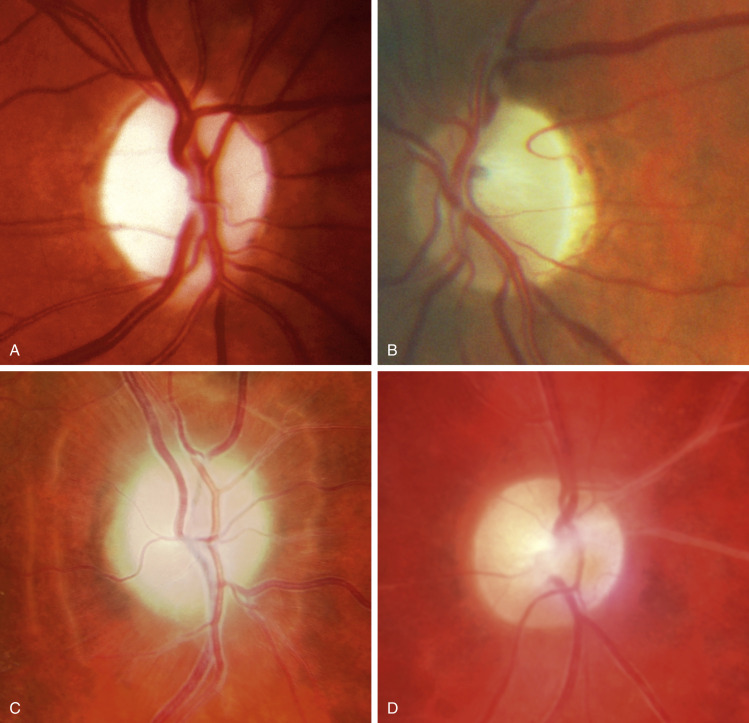
- Optic disc pallor (Fig. E1) occurs 4 to 6 wk after optic nerve insult.
- Unilateral lesion produces a relative afferent pupillary defect (RAPD): When swinging flashlight eye to eye, the abnormal pupil dilates to direct light.
- Decreased visual acuity, blurred vision, visual field deficits (e.g., central scotoma), abnormal color vision (e.g., red desaturation).
(A) Primary due to compression. (B) Primary due to nutritional neuropathy-note predominantly temporal pallor. (C) Secondary due to chronic papilledema-note prominent Paton lines. (D) Consecutive due to vasculitis.
Courtesy P. Gili, Fig. C. From Bowling B: Kanski’s clinical ophthalmology: a systemic approach, ed 8, Philadelphia, 2016, Elsevier.
- Inflammatory optic neuritis: MS, sarcoidosis, neuromyelitis spectrum disorder, infections (syphilis, CMV, HIV, Lyme disease, cat-scratch disease)
- Vascular: Arteritic and nonarteritic ischemic optic neuropathy, central retinal artery occlusion, temporal arteritis, diabetes
- Compression: Pituitary, orbital, or other tumors, idiopathic intracranial hypertension, meningioma, thyroid eye disease
- Hereditary: Leber hereditary optic neuropathy, autosomal dominant optic atrophy, leukodystrophies, other mitochondrial diseases.
- Nutritional, toxic, and metabolic: Amiodarone, isoniazid, tacrolimus, ethambutol, linezolid, vigabatrin, B12 deficiency, folate deficiency, copper deficiency, methanol, tobacco, alcohol1
- Trauma
- Radiation
- Glaucoma (end-stage disease)