AUTHOR: R. Scott Hoffman, MD
The term conjunctivitis refers to an inflammation of the conjunctiva resulting from a variety of causes, including allergies and bacterial, viral, and chlamydial infections.
Pseudomembranous conjunctivitis
| ||||||||||||||||||||||||
- Allergic conjunctivitis (Fig. E1), the most common form of ocular allergy, is usually associated with allergic rhinitis and may be seasonal or perennial.
- Bacterial or viral conjunctivitis is often seasonal and can be extremely contagious.
Occurs at any age. Most cases in adults are due to viral infection. Children are more prone to develop bacterial conjunctivitis than viral forms. Table E1 summarizes manifestations of acute conjunctivitis in children
TABLE E1 Manifestations of Acute Conjunctivitis in Children
| FEATURE | CLINICAL CHARACTERISTICS | |
|---|---|---|
| BACTERIAL | VIRAL | |
| Common pathogens | Haemophilus influenzae (usually nontypable) | Adenoviruses types 8, 19 |
| Streptococcus pneumoniae | Enteroviruses | |
| Moraxella catarrhalis | Herpes simplex virus | |
| Incubation | 24-72 h | 1-14 days |
| SYMPTOMS | ||
| Photophobia | Mild | Moderate to severe |
| Blurred vision | Common with discharge | If keratitis is present |
| Foreign body sensation | Unusual | Yes |
| SIGNS | ||
| Discharge | Purulent discharge | Mucoid/serous discharge |
| Palpebral reaction | Papillary response | Follicular response |
| Preauricular lymph node | Unusual for acute (<10%) | More common (20%) |
| Chemosis | Moderate | Mild |
| Hemorrhagic conjunctivae | Occasionally with pneumococcus or Haemophilus sp. | Frequent with enteroviruses |
| Treatment (topical) | Polymyxin B-trimethoprim orsulfacetamide 5% or erythromycin or moxifloxacin or gatifloxacin | Adenovirus: Self-limited Herpes simplex virus: Trifluridine 1% solution or ganciclovir 0.15% gel or acyclovir; ophthalmologic consultation |
| End of contagious period | 24 h after start of effective treatment | 7 days after onset of symptoms |
From Marcdante KJ et al: Nelson essentials of pediatrics, ed 9, Philadelphia 2023, Elsevier.
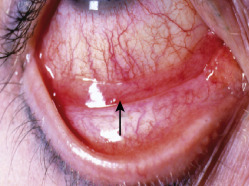
- Infection and chemosis of conjunctivae with discharge. Gluing of the eyelids and no itching is more indicative of a bacterial cause (Fig. E2).
- Cornea is clear or can be involved (certain bacteria, such as Neisseria, can rapidly develop into corneal infection).
- Vision is often normal but can be blurred. Mucus and watering can cause fluctuating vision.
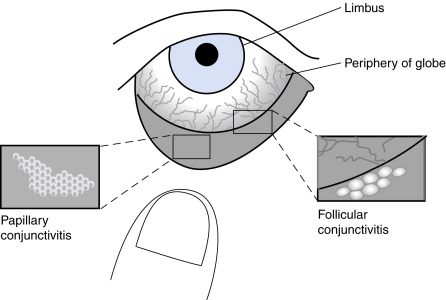
- Fig. E3 illustrates the difference between papillary and follicular conjunctivitis.
Figure E2 Bacterial conjunctivitis.
Purulent discharge and conjunctiva hyperemia suggest bacterial conjunctivitis. Viral conjunctivitis produces watery discharge, foreign body sensation, preauricular lymphadenopathy, and conjunctival follicles seen on slit lamp examination.
Reproduced with permission from the American Academy of Ophthalmology. From Goldman L, Schafer AI: Goldman’s Cecil medicine, ed 24, Philadelphia, 2012, Saunders.
Figure E3 Conjunctivitis: Papillary versus follicular.
The erythema of conjunctivitis (shaded dark gray) is most intense on the inside surface of the eyelids (tarsal conjunctiva) and peripherally on the globe (near the fornices), whereas the erythema is less intense centrally near the limbus. In more severe conjunctivitis, the entire conjunctival surface (both tarsal and bulbar) is red. This pattern of erythema contrasts with iritis, which causes more intense erythema centrally around the limbus, a finding called circumlimbal flush or ciliary flush. In patients with conjunctivitis, the clinician should inspect the everted upper or lower lids, noting whether the inner membrane has its normal smooth surface or instead has small, uneven projections, which are characterized as either papillae or follicles. In this example, the clinician has used his thumb to gently evert the lower lid for inspection. Papillae (left bottom) are contiguous red vascular bumps; the center of each papilla contains a blood vessel. They are red on the surface and pale at the base. Papillae are often so tiny that the conjunctiva acquires a velvety appearance, and only magnification reveals their true nature. Other times, papillae may become large and produce a cobblestone appearance. Follicles (right bottom) are discrete 1- to 2-mm-diameter white bumps consisting of aggregates of lymphoid tissue; the center of each is avascular. They are pale on the surface and red at the base.
From McGee S: Evidence-based physical diagnosis, ed 4, Philadelphia, 2018, Elsevier.
- Bacterial: Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis in children; Staphylococcus spp in adults. Gram-negative infections are more common in contact lens wearers. Gonococcal ophthalmia neonatorum is caused by Neisseria gonorrhoeae acquired by exposure of the neonatal conjunctivae to infected cervicovaginal secretions during delivery
- Viral: Most common overall cause of infectious conjunctivitis
- Chlamydial
- Allergic
- Traumatic (chemical or toxin exposure)
- Chronic eyelid inflammation (blepharitis)