AUTHOR: Joseph S. Kass, MD, JD, FAAN



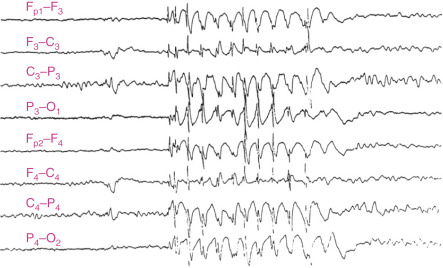
DefinitionAbsence seizures are a type of generalized seizure characterized by brief episodes of staring with impairment of consciousness (absence). They usually last no more than 20 to 30 sec. The onset and the end of the seizures are sudden. Patients are typically unaware of the seizure and resume the activity they were performing before the seizure. The electroencephalogram signature of absence seizures consists of a generalized 3-Hz spike and slow wave discharges.
SynonymsChildhood absence epilepsy
Seizures, absence
| ICD-10CM CODE | | G40.309 | Generalized idiopathic epilepsy and epileptic syndromes, not intractable, without status epilepticus |
|
Epidemiology & DemographicsIncidence1 to 10 cases per 100,000 population
PrevalenceRepresents up to 18% of all pediatric epilepsy syndromes
Predominant Sex and AgeMore common in girls than in boys, absences typically begin between 4 and 10 yr and remit by age 201
Physical Findings & Clinical Presentation
- Patients with absence seizures usually have normal physical and neurologic examinations.
- During the seizures, the patients are unresponsive and can have motor phenomena (automatisms, eye blinks, mouth and hand movements).
- Absence seizures are not associated with post-ictal confusion.
- They may be triggered by hyperventilation associated with activity.
- Tonic clonic seizures are not usually a feature of this syndrome. If the patient also experiences tonic clonic seizures, other etiologies should be investigated, such as juvenile absence epilepsy, juvenile myoclonic epilepsy, complex partial seizures, etc.

The medication of choice based on the best current evidence available is ethosuximide, followed by valproic acid and lamotrigine.2
Nonpharmacologic TherapyNot applicable
Acute General Rx
- Ethosuximide: Initial dose: 10 mg/kg/day; then after 7 days, 20 mg/kg
- Divalproex sodium (Depakote): Initial dose: 5 to 10 mg/kg/day (divided bid), maximum dose: 60 mg/kg/day
- Lamotrigine (Lamictal): Dose for patients on no other antiepileptic drugs. Wk 1 and 2: 0.3 mg/kg/day. Wk 3 and 4: 0.6 mg/kg/day. Wk 5 onward: Increase every 1 to 2 wk by 0.6 mg/kg/day. Maintenance: 4.5 to 7.5 mg/kg/day. Warning: Should be used with caution due to the potential for toxicity and Stevens-Johnson syndrome. Patients on other antiepileptic drugs can also have severe adverse reactions (e.g., valproate can cause increased levels of lamotrigine, and lamotrigine must be titrated much more slowly in patients on valproate therapy)
Chronic Rx
- Children with recurrent seizures require chronic treatment.
- If children are seizure-free for a period of 1 to 2 yr, a trial on no medications should be considered; children typically outgrow childhood absence seizures.
Disposition
- Response to treatment is excellent.
- Absence seizures tend to remit in teenage yr.
- Epilepsy can be considered as resolved once 10 yr have elapsed since the last event, including 5 yr free from medications.
Complementary & Alternative MedicineNot applicable
ReferralPatients with epilepsy should be referred for a consultation by a child neurologist, preferably one specializing in epilepsy.