AUTHORS: Meredith Carrel-Lammert, MD and Jennifer Yeung, DO


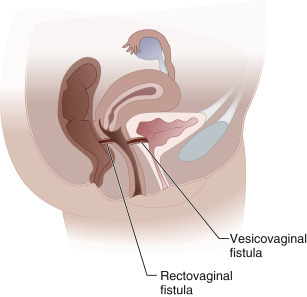
DefinitionVaginal fistula is an abnormal passageway between the vagina and another epithelialized surface (Fig. E1).
| ICD-10CM CODES | | N82.0 | Vesicovaginal fistula | | N82.2 | Fistula of vagina to small intestine | | N82.3 | Fistula of vagina to large intestine | | N82.9 | Female genital tract fistula, unspecified |
|
Figure E1 The Two Most Common Types of Vaginal Fistulas are Vesicovaginal and Rectovaginal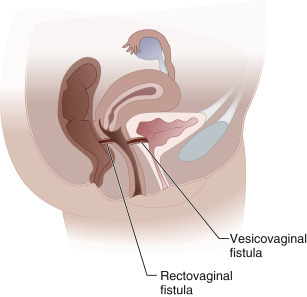
From Fielding JR et al: Gynecologic imaging, Philadelphia, 2011, Saunders.
Epidemiology & DemographicsIncidenceAfter benign hysterectomy: <1% (0.08% to 0.26%); after radical hysterectomy: 1% to 4%. Incidence is difficult to estimate in developing countries because of lack of medical care and medical follow-up after obstetric care.1
PrevalenceRare in the developed world from obstetric complications, but in developing countries, the best estimate of prevalence is as high as 124 in 100,000.2
Risk Factors3,4In developing countries:
- Obstetric trauma
- Prolonged, protracted labor
- Cephalopelvic disproportion causing ischemia and necrosis of the tissue between the fetal head and maternal pubic bone
In developed countries:
- Hysterectomy, especially with the following:
- Extensive bladder dissection
- Iatrogenic injury of the bowel, bladder, or ureters
- Prolonged operating times (>5 hr)
- Laparoscopic approach has the greatest risk, vaginal approach the lowest
- Large blood loss
- Large volume uterus (>250 g)
- Coexisting pelvic adhesions distorting the normal pelvic anatomy
- Obstetric trauma:
- Rectovaginal fistulas are primarily related to severe vaginal lacerations. Risk factors for such include:
- Primiparity
- Midline episiotomies
- Increasing birth weights
- Use of vaginal forceps
- Bladder injury related to uterine rupture
- Invasive cancer
- Pelvic radiation, directly proportional to dosimetry:
- Also as a result of tumor necrosis after therapy
- Chronic inflammatory disease:
- Crohn disease-up to 7% of patients will develop fistula formation
- Diverticulitis
- Pelvic infection:
- Tuberculosis
- Syphilis
- Lymphogranuloma venereum
- Trauma
- Previous pelvic surgery
- Diabetes mellitus
- Age >50, likely as a result of poor tissue quality from menopausal estrogen deficiency, although some studies have refuted this
- Tobacco usage
- Foreign bodies:
- Suburethral slings for stress urinary incontinence have increased the incidence of urethrovaginal fistula
- Unmaintained pessary
Physical Findings & Clinical Presentation
- Flatus, stool, or urine per vagina
- Frequent urinary tract infections
- Urinary odor, hematuria
- Mucopurulent malodorous discharge per vagina
- Dyspareunia
- Perineal pain, perineal dermatitis
- Recurrent vaginal infections
Etiology (Box E1
- Obstetric:
- Incompletely repaired or unidentified vaginal lacerations
- Prolonged pressure between the fetal head and the maternal pubic bone, causing tissue necrosis
- Gynecologic:
- Extensive dissection about the urinary tract, including unidentified injury
- Poor-quality tissue with prolonged healing as a result of estrogen deficiency, infection, malignancy, or prior radiation therapy
- Gastrointestinal:
- Crohn disease. Transmural bowel inflammation is associated with sinus tracts that can lead to fistula formation.5 In population-based study of 169 patients with Crohn disease, 7% had evidence of fistula 30 days prior to diagnosis of the disease.6
BOX E1 Etiology of Vesicovaginal Fistula
Traumatic - Postsurgical
- Abdominal hysterectomy
- Vaginal hysterectomy
- Anti-incontinence surgery
- Anterior vaginal wall prolapse surgery (e.g., colporrhaphy)
- Vaginal biopsy
- Bladder biopsy, endoscopic resection, laser therapy
- Other pelvic surgery (e.g., vascular, rectal)
External trauma (e.g., penetrating, pelvic fracture, sexual) - Radiation therapy
- Advanced pelvic malignancy
- Infectious or inflammatory cause
- Foreign body
- Obstetric
- Obstructed labor
- Forceps laceration
- Uterine rupture
- Cesarean section injury to bladder
- Congenital
|
From Wein AJ et al: Campbell-Walsh urology, ed 11, Philadelphia, 2016, Elsevier.

Prevention
- Prompt repair of obstetric lacerations.
- Screen patients most at risk for complications before surgery.
- Avoid urologic complications in surgery (e.g., injury to bladder or ureters).
- Perform cystoscopy with complicated hysterectomy dissections to identify defects immediately.
- Close management of inflammatory diseases like Crohn disease.
Nonpharmacologic Therapy7- Tension-free surgical repair, with multiple documented approaches (Table E1):
- Transvaginal
- Perineal
- Abdominal
- Laparoscopic
- Robot assisted
- Transrectal
- Transanal endoscopy
- If vesicovaginal fistula is small (<1 cm) and identified early:
- Prolonged urinary catheter placement, greater than 3 wk
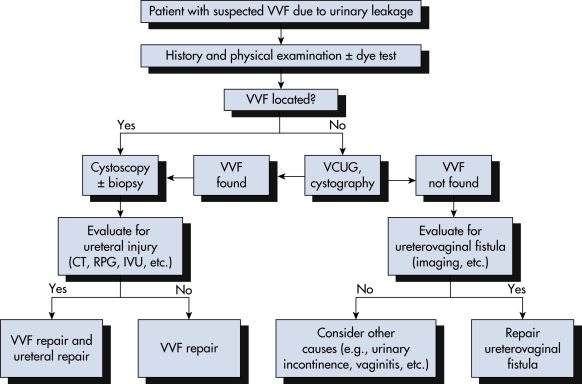
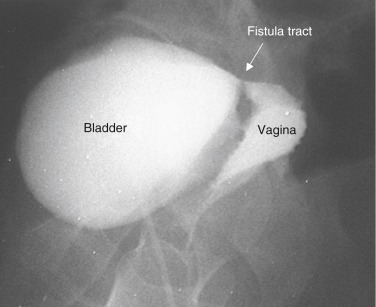
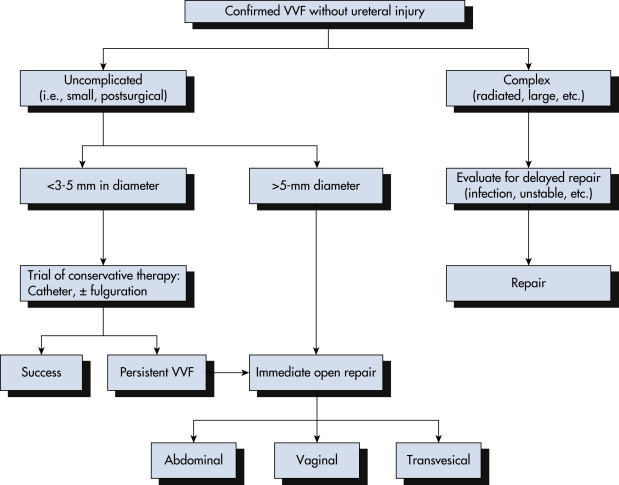
Figure E5 Algorithm for management of vesicovaginal fistula (VVF).
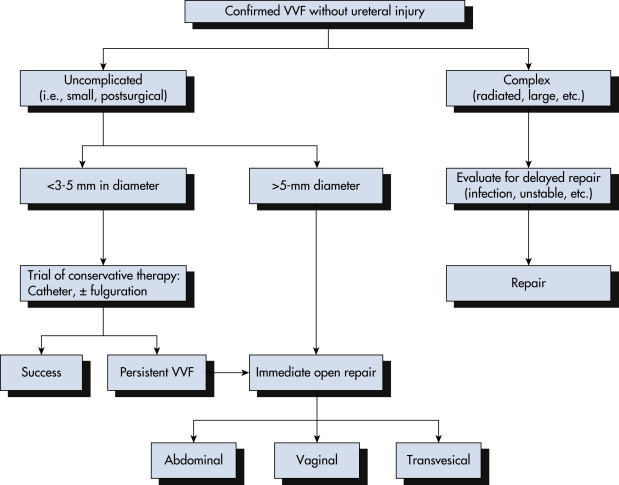
From Wein AJ et al: Campbell-Walsh urology, ed 11, Philadelphia, 2016, Elsevier.
TABLE E1 Abdominal Versus Transvaginal Repair of Vesicovaginal Fistula
| Abdominal | Transvaginal |
|---|
| Incision | Abdominal incision | Vaginal incision(s) can be done immediately in the absence of infection or other complications. |
| Timing of repair (elapsed time from fistula creation) | Often delayed 3-6 mo. |
| Exposure | Fistula located low on the trigone or near the bladder neck may be difficult to expose transabdominally. | Fistula located high at the vaginal cuff may be difficult to expose transvaginally. |
| Location of ureters relative to fistula tract | Fistula located near ureteric orifice may necessitate reimplantation. | Reimplantation may not be necessary even if fistula tract is located near ureteric orifice. |
| Sexual function | No change in vaginal depth. | Risk of vaginal shortening (e.g., Latzko technique). |
| Use of adjunctive flaps | Omentum, peritoneal flap, rectus abdominis flap. | Labial fat pad (Martius fat pad), peritoneal flap, gluteal skin, or gracilis myocutaneous flap. |
| Relative indications | Large fistulae, location high in a deep narrow vagina, radiation fistulae, failed transvaginal approach, small-capacity bladder requiring augmentation, need for ureteral reimplantation, inability to place patient in the lithotomy position. | Uncomplicated fistulae, low fistulae. |
From Wein AJ et al: Campbell-Walsh urology, ed 11, Philadelphia, 2016, Elsevier.
Acute General Rx- Treatment of urinary or vaginal infection
- Estrogen replacement therapy, local vs. systemic if no contraindications
- Surgical repair of fistula with subsequent pelvic rest for 4 to 6 wk
- Minimizing Valsalva maneuvers
- Treatment of proctitis and obtain control of Crohn disease prior to any attempts at surgical intervention.
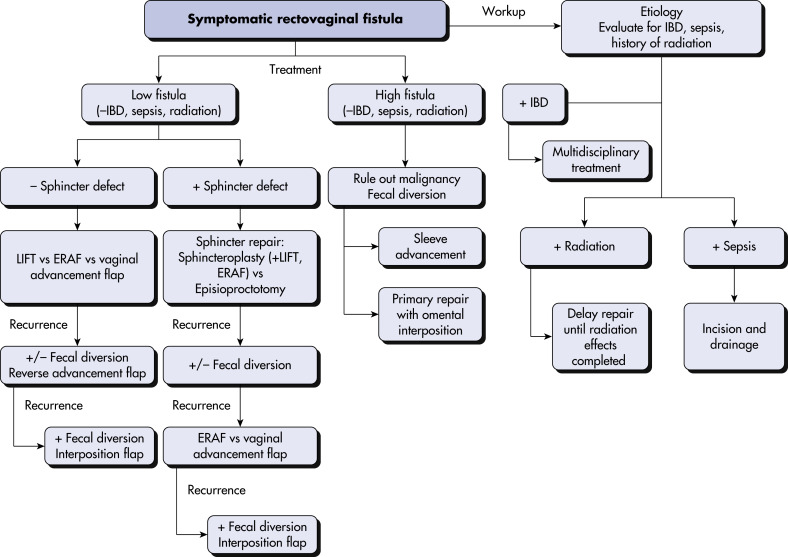
- Fig. E6 illustrates a treatment algorithm for primary and recurrent rectovaginal fistulas
Figure E6 Proposed treatment algorithm for primary and recurrent rectovaginal fistula.
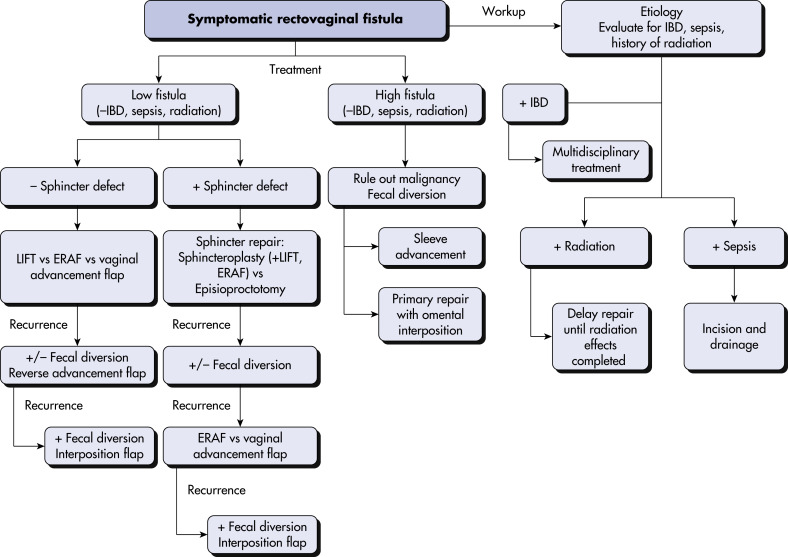
ERAF, Endorectal advancement flap; IBD, inflammatory bowel disease; LIFT, ligation of the intersphincteric fistula tract.
From Cameron JL, Cameron AM: Current surgical therapy, ed 12, Philadelphia, 2017, Elsevier.
Chronic RxIf initial surgical management fails, repeat operations tailored to the cause of the fistula would be indicated, such as advancement flaps, sphincteroplasty, coloanal anastomosis (for rectovaginal fistula), gracilis flap. A 10-yr retrospective cohort study from the English National Health Service inpatient database showed that 11.9% of patients required repeat operations.
DispositionCure rates after surgical repair vary in the literature, especially with the type of fistula repaired. With early intervention, estimated cure rates are between 84% and 100% in developed countries.
ReferralIf there is concern for vaginal fistula, the patient should be managed by a surgeon familiar with fistula surgery for repair and follow-up. Consider consulting with a urologist, colon and rectal surgeon, gynecologic oncologist, or urogynecologist.