AUTHOR: Katherine Elizabeth McGraw, MD
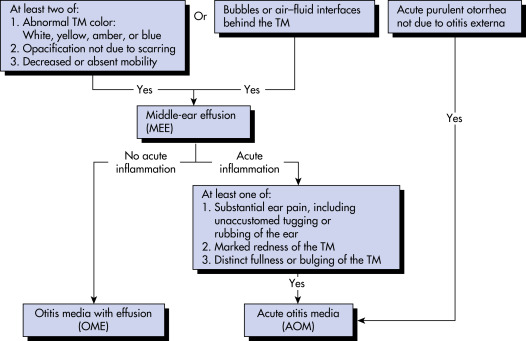
Acute otitis media (AOM) is defined by infected middle ear fluid resulting in moderate to severe bulging of the tympanic membrane (TM) or new onset of otorrhea not due to acute otitis externa. Table 1 summarizes otitis media definitions and terminology. Care should be taken to differentiate AOM from serous otitis media, which involves noninfected middle ear fluid that does not result in bulging of the TM. Serous otitis media does not require antibiotic treatment.1,2
TABLE 1 Otitis Media Definitions and Terminology
| Preferred Term | Definition | Comment |
|---|---|---|
| Otitis media (OM) | Inflammation of the middle ear without reference to etiology or pathogenesis | Nonspecific umbrella term for any condition associated with middle ear inflammation |
| Acute otitis media (AOM) | Rapid onset of signs and symptoms of inflammation in the middle ear | Diagnosed when there is moderate to severe bulging of the ear drum; mild bulging of the ear drum and recent (<48 h) onset of ear pain or intense erythema of the ear drum; or acute ear discharge unrelated to otitis externa (inflammation of the external ear canal)∗ |
| Recurrent AOM (rAOM) | ≥3 well-documented and separate AOM episodes in the preceding 6 mo or ≥4 episodes in the preceding 12 mo with >1 episode in the past 6 mo | Children without persistent MEE tend to have a good prognosis and often improve spontaneously; children with persistent MEE have a poorer prognosis and might benefit from ventilation tubes |
| Otitis media with effusion (OME) | Fluid in the middle ear without signs or symptoms of acute ear infection | Diagnosed by one or more of the following: Reduced ear drum mobility on pneumatic otoscopy, reduced ear drum mobility on tympanometry, opaque ear drum or a visible air-fluid interface behind the ear drum on otoscopy |
| Chronic OME | OME persisting for ≥3 mo from date of onset (if known) or from date of diagnosis (if onset is unknown) | Chronic OME has much lower rates of spontaneous resolution compared to OME of new onset or following an episode of AOM |
| Chronic suppurative otitis media (CSOM) | Chronic inflammation of the middle ear and mastoid mucosa with a nonintact ear drum (perforation or ventilation tube) and persistent ear discharge | No consensus on duration of ear discharge needed for diagnosis, with recommendations ranging from 2 wk to at least 3 mo |
| Middle ear effusion (MEE) | Fluid in the middle ear from any cause | MEE is present with both OME and AOM and might persist for weeks or months after the signs and symptoms of AOM resolve |
∗The degree of bulging does not reflect AOM severity. Severe AOM is defined as having moderate-to-severe ear pain, ear pain for at least 48 h, or temperature 39° C or higher.
From Flint PW et al: Cummings otolaryngology, head and neck surgery, ed 7, Philadelphia, 2021, Elsevier.
Acute suppurative otitis media
| ||||||||||||||||||||||||||||
- Affects patients of all ages but is largely a disease of infants and young children
- Affects approximately 80% of all children by age 5 yr
- Occurs three or more times in one third of all children by age 3 yr
- Costs associated with otitis media exceed $5 billion, with 40% of the costs occurring from patients ages 1 to 3 yr
- One of the most common indications for antibiotic prescription among children
- AOM occurs at all ages but is most prevalent between 6 and 24 mo of age.
- A second peak in incidence occurs between 4 and 6 yr of age.
- AOM is most frequent in the fall, winter, and early spring (coincident with peak respiratory virus prevalence in the community).
- Incidence of infection declines with age; AOM is seen infrequently in adults.
- Moderate to severe bulging of the TM.
- Fluid in the middle ear along with signs and symptoms of local inflammation.
- Erythema with diminished light reflex (Fig. E1)
- As infection progresses, middle ear exudation occurs (exudative phase); the exudate rapidly changes from serous to purulent (suppurative phase).
- Retraction and poor mobility of the TM ensues, and the TM begins to bulge.
- At any time during the suppurative phase, the TM may rupture, releasing the middle ear contents (otorrhea).
- Erythema of the TM without other abnormalities is not a diagnostic criterion for acute otitis media (AOM) because it may occur with any inflammation of the upper respiratory tract, crying, or nose blowing.
- Symptoms1:
- Rapid- or recent-onset otalgia, ranging from slight discomfort to severe, is the most common presenting symptom.
- Hearing loss while middle ear fluid is present.
- Otorrhea (if TM has ruptured).
- Systemic symptoms such as fever, listlessness, irritability, decreased appetite, vomiting, and diarrhea are common. Although vertigo, facial swelling, nystagmus, tinnitus, lethargy, and facial nerve palsies can occur as rare complications of AOM; these symptoms should prompt consideration of an alternate diagnosis.
- Table 2 summarizes symptom scoring systems designed to aid in diagnosis.
- After an episode of AOM:
- Persistence of effusion for weeks or months (called secretory, serous, or nonsuppurative otitis media)
- Fever and otalgia usually absent
- Hearing loss possible (10 to 50 dB, with predominant involvement of the low frequencies)
- Manifestations of the sequelae and complications of otitis media are summarized in Table E3
TABLE 2 Acute Otitis Media Symptom Scoring Systems Designed to Aid in Diagnosis
| 3-Item Otitis Media Score (OM-3) | Ear Treatment Group Symptom Questionnaire (ETG-5) | Acute Otitis Media Faces Scale (AOM-FS) | Otoscopic Severity Scale (OS-8) | Acute Otitis Media Severity of Symptom Scale (AOM-SOS) | Otitis Media Clinical Severity Index (OM-CSI) 30-Point Scalea | Otitis Media Clinical Severity Index (OM-CSI) 10-Point Scalea |
|---|---|---|---|---|---|---|
| Physical suffering | Ear pain | Seven facial expressions ranging from no problem to extreme problem | Eight categories of TM inflammationb | Ear pain | Ear pain | Ear pain |
| Emotional distress | Fever | Ear tugging | Fever | Fever | ||
| Limitation of activities | Irritability | Irritability | Irritability | Irritability | ||
| Appetite | Decreased play | Fever at examination | Fever at examination | |||
| Sleep quality | Decreased appetite | TM erythema | TM erythema | |||
| Difficulty sleeping | TM mobility | TM mobility | ||||
| Fever | TM position | TM position | ||||
| Effusion color | Effusion color | |||||
| Otorrhea | Otorrhea |
TM, Tympanic membrane.
a The 30-point scale used a 2- to 5-point Likert scale and the 10-point scale used a 2- to 3-point Likert scale.
b 0 = normal; 1 = erythema only; 2 = erythema, air-fluid level, clear fluid; 3 = erythema, complete effusion, no opacification; 4 = erythema, opacification with air-fluid level or air bubbles, no bulging; 5 = erythema, complete effusion, opacification, no bulging; 6 = erythema, bulging rounded doughnut appearance of the tympanic membrane; 7 = erythema, bulging, complete effusion and opacification with bulla formation.
From Cherry JD et al: Feigin and Cherry’s pediatric infectious diseases, ed 8, Philadelphia, 2019, Elsevier.
A, Normal tympanic membrane with pearly gray, translucent appearance. B, OME with air bubbles. C and D, OME fully filled with effusion; note retracted and translucent tympanic membrane with prominent head of the malleus. E, Slight bulging with semiopaque white tympanic membrane. F, Bulging semiopaque tympanic membrane. G, Markedly bulging, donut appearance, opaque, white tympanic membrane. H and I, Severe bulging with bullae formation.
Courtesy Dr. Hoberman, University of Pittsburgh. In Cherry JD et al: Feigin and Cherry’s pediatric infectious diseases, ed 8, Philadelphia, 2019, Elsevier.
TABLE E3 Manifestations of the Sequelae and Complications of Otitis Media
| Complication | Clinical Features | ||
|---|---|---|---|
| Acute | |||
| Perforation with otorrhea | Immobile tympanic membrane secondary to visible perforation, exudate in ear canal | ||
| Acute mastoiditis with periostitis | Tenderness and erythema over mastoid process, no destruction of bony trabeculae | ||
| Acute mastoid osteitis | Destruction of bony trabeculae; tenderness and erythema over mastoid process coupled with outward displacement of pinna | ||
| Petrositis | Infection of perilabyrinthine cells; may present with otitis, paralysis of lateral rectus, and ipsilateral orbital or facial pain (Gradenigo syndrome) | ||
| Facial nerve palsy | Peripheral cranial nerve VII paralysis | ||
| Labyrinthitis | Vertigo, fever, ear pain, nystagmus, hearing loss, tinnitus, nausea and vomiting | ||
| Lateral sinus thrombosis | Headache, fever, seizures, altered states of consciousness, septic emboli | ||
| Meningitis | Fever, headache, nuchal rigidity, seizures, altered states of consciousness | ||
| Intracranial empyema or brain abscess | Fever, headache, seizures, altered states of consciousness, focal neurologic examination findings | ||
| Nonacute | |||
| Chronic perforation | Immobile tympanic membrane secondary to perforation | ||
| Otitis media with effusion (OME) | Immobile, opaque tympanic membrane | ||
| Adhesive otitis | Irreversible conductive hearing loss secondary to chronic OME | ||
| Tympanosclerosis | Thickened white plaques may cause conductive hearing loss | ||
| Chronic suppurative otitis media | Following acute otitis media with perforation, secondary infection with Staphylococcus aureus, Pseudomonas aeruginosa, or anaerobes develops, causing chronic otorrhea | ||
| Cholesteatoma | White, pearl-like, destructive tumor with otorrhea arising near or within tympanic membrane; may be secondary to chronic negative middle ear pressure | ||
| Otitic hydrocephalus | Increased intracranial pressure secondary to AOM; signs and symptoms include severe headaches, blurred vision, nausea, vomiting, papilledema, diplopia (abducens paralysis) | ||
AOM, Acute otitis media.
From Kliegman RM: Nelson textbook of pediatrics, ed 21, Philadelphia, 2020, Elsevier.
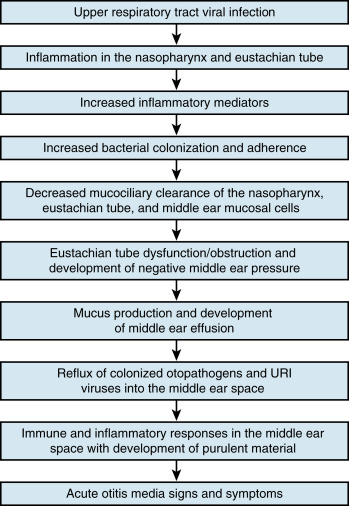
- Most common etiology is a viral upper respiratory tract infection, which causes inflammation and dysfunction of the eustachian tube and transient aspiration of nasopharyngeal secretions into the middle ear (Fig. 2). Bacterial colonization from the nasopharynx in conjunction with eustachian tube dysfunction leads to infection.
- May occasionally develop as a result of hematogenous spread or by direct invasion from the nasopharynx.
- Conjugated pneumococcal vaccination of children has resulted in decreases in Streptococcus pneumoniae causing AOM.
- Most common bacterial pathogens4,5:
- Of increasing importance, infection caused by penicillin-nonsusceptible S. pneumoniae (MIC >0.1 mg/ml), ranging from 8% to 34%. About 50% of PNSSP isolates are penicillin-intermediate (MIC 0.1 to 2.0 mg/ml).
- Group A streptococci is associated with higher rates of TM perforation than AOM caused by other pathogens.
- Viral pathogens:
- Others: