AUTHOR: Glenn G. Fort, MD, MPH
Definition
Cholangitis refers to an inflammation and/or infection of the hepatic and common bile ducts associated with obstruction of the common bile duct.
Physical Findings & Clinical Presentation
- Usually acute onset of fever, abdominal pain (RUQ), and jaundice (Charcot triad)
- All signs and symptoms in only 50% to 85% of patients
- Often, dark coloration of the urine resulting from bilirubinuria
- Complications:
- Bacteremia (50%) and septic shock
- Hepatic abscess and pancreatitis
Etiology
Obstruction of the common bile duct causing rapid proliferation of bacteria in the biliary tree
- Most common cause of common bile duct obstruction: Stones, usually migrated from the gallbladder
- Other causes: Prior biliary tract surgery with secondary stenosis, tumor (usually arising from the pancreas or biliary tree), and parasitic infections from Ascaris lumbricoides or Fasciola hepatica
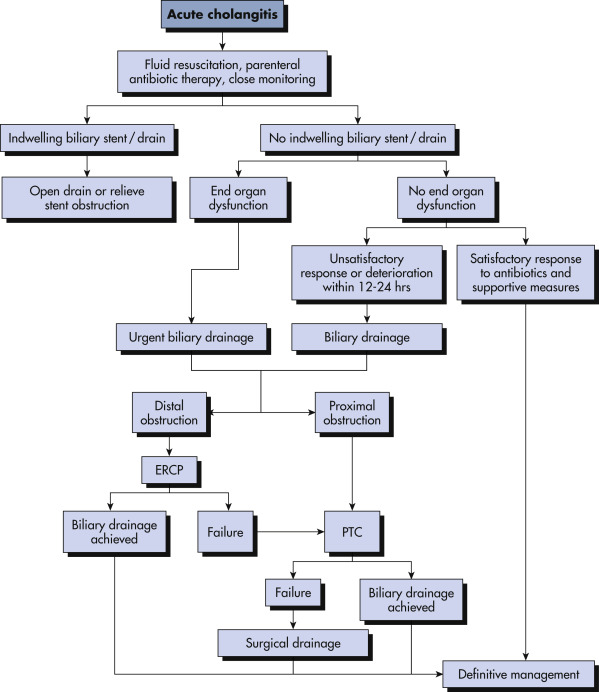
- Iatrogenic after contamination of an obstructed biliary tree by endoscopic retrograde cholangiopancreatoscopy (ERCP) or percutaneous transhepatic cholangiography (PTC)
- Primary sclerosing cholangitis (PSC)
- HIV-associated sclerosing cholangitis: Associated with infection by cytomegalovirus, Cryptosporidium, Microsporidia, and Mycobacterium avium complex