Nonpharmacologic TherapyCerclage has long been the mainstay of treatment for cervical insufficiency (Fig. E1 to E3 to ). However, randomized controlled trials (RCTs) comparing the rates of preterm birth in patients receiving cervical cerclage vs. those without cerclage have produced conflicting results, with many studies showing little or no improvement in preterm birth rates. The greatest benefit of cerclage is in women with singleton pregnancies who have experienced a previous preterm birth, and cerclage is actually detrimental to women carrying multiple gestations. The most common risk associated with cerclage is cervical laceration during delivery (1% to 13%). Bed rest is often used when there is a threat of preterm birth, although its benefit is not proven and it has detrimental effects for the mother, such as venous thromboembolic events; thus it is not recommended.
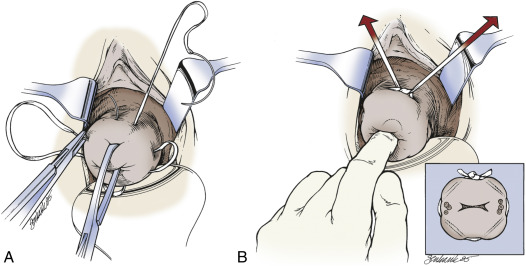
Figure E1 Placement of sutures for McDonald cerclage.
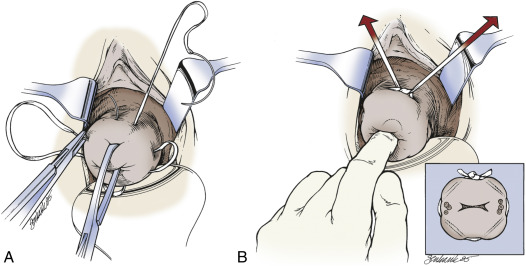
A, We use a double-headed Mersilene band with four bites in the cervix, avoiding the vessels. B, The suture is placed high up in the cervix, close to the cervicovaginal junction, approximately at the level of the internal os.
From Gabbe SG: Obstetrics, ed 6, Philadelphia, 2012, Saunders.
Figure E2 Transvaginal sonogram of the cervix after cerclage placement.

The internal os is closed, and there is no funneling. Echogenic spots in the cervix correspond to cerclage (arrows).
From Gabbe SG: Obstetrics, ed 6, Philadelphia, 2012, Saunders.
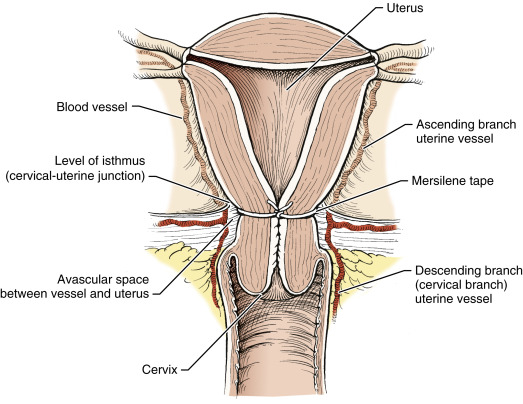
Figure E3 Abdominal cerclage.
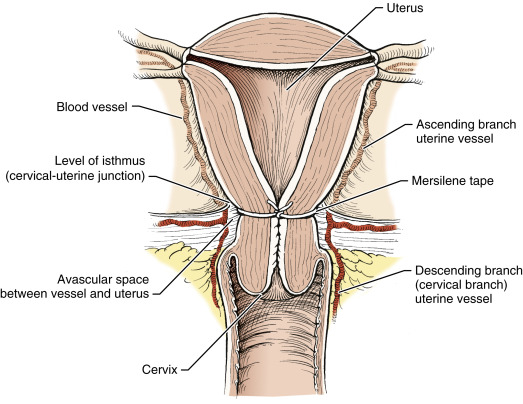
Surgical placement of circumferential Mersilene tape around uterine isthmus and median to uterine vessels. Knot is tied anteriorly.
From Gabbe SG: Obstetrics, ed 6, Philadelphia, 2012, Saunders.
Acute General RxUltrasound-indicated cerclage should be placed in women with ultrasonographic evidence of cervical shortening (<25 mm) before 24 wk gestation and a history of a preterm birth before 34 wk. Women who present with painless cervical dilation in the second trimester may be candidates for a physical-examination-indicated cerclage (rescue cerclage) after being ruled out for uterine activity and evidence of infection. Data are limited on the efficacy of placing a physical-examination-indicated cerclage. Women should be counseled about the potential risks of rescue cerclage in the setting of unclear benefit. Placement of a cervical pessary is only currently recommended in the setting of research trial protocols.
Chronic RxProphylactic cerclage (history-indicated cerclage) has been shown by several studies and meta-analyses to be most heavily indicated in women with prior history of multiple preterm births. Women with a history of one or more second-trimester deliveries with no symptoms or signs of labor at the time of the delivery may be candidates for a prophylactic cerclage, placed at 13 to 14 wk gestation. Women with this history should also be offered 17-OH progesterone injections between 16 and 36 wk.
DispositionPatients with a singleton pregnancy, prior history of preterm birth, and shortened cervix (<25 mm) on transvaginal ultrasound should be counseled regarding amniocentesis and cerclage placement.
Related ContentCervical Incompetence (Patient Information)
Preterm Labor (Related Key Topic)
Premature Rupture of the Membranes (Related Key Topic)