|
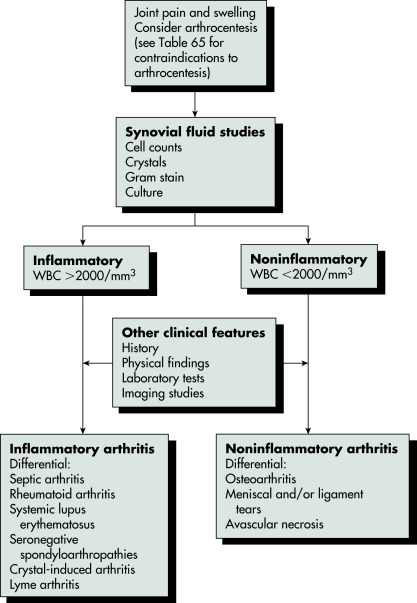
Figure 112 Diagnostic approach for swollen joints.

WBC, White blood cell count.
From Goldman L, Schafer AL [eds]: Cecil textbook of medicine, ed 24, Philadelphia, 2012, Saunders.
Table 64 Clinical and Radiologic Findings in Joint Disease
| Condition | Site of Involvement | Discriminatory Findings |
|---|---|---|
| Primary osteoarthritis (F>M •>45 yr) | Hands | PIP and DIP joint involvement (Heberden and Bouchard nodes) |
| Large joints (e.g., hip, knee) | Joint space narrowing | |
| Spine | Degenerative disc disease | |
| Erosive osteoarthritis (affects middle-aged females) | Hands | PIP and DIP joint involvement |
| Rheumatoid arthritis (F>M • Rh factor positive) | Hand and wrist | Symmetric arthritis |
| Large joints | Joint space narrowing | |
| Spine | Atlantoaxial subluxation | |
| Juvenile idiopathic arthritis (M = F • affects children) | Hands | Joint ankylosis |
| Large joints (e.g., knee) | Abnormalities of growth and maturation | |
| Cervical spine | Apophyseal joint fusion | |
| Psoriatic arthritis (M>F •nail changes • HLA-B27 +ve) | Upper extremities (e.g., hands) | “Sausage” digit |
| SI joints | Asymmetric or unilateral sacroiliitis | |
| Spine | Coarse syndesmophytes | |
| Reites syndrome (affects young male adults) | Lower extremities (e.g., foot) | Hallux involvement |
| Spine | Coarse syndesmophytes | |
| SI joints | Asymmetric or unilateral sacroiliitis | |
| Ankylosing spondylitis (M>F • affects young adults • HLA-B27 +ve in 95%) | SI joints | Bilateral symmetric sacroiliitis |
| Spine | Anterior vertebral body squaring | |
| Pelvis | “Whiskering” of the iliac crests and ischial tuberosities | |
| Enteropathic arthropathies | SI joints | Symmetric sacroiliitis |
| Gout (M>F) | Hands and feet (especially the great toe) | MTP joint of the great toe |
| CPPD crystal deposition disease (M = F) | Any peripheral joint | Degenerative changes |
| HA crystal deposition disease (M = F) | Predilection for the shoulder (supraspinatus tendon) | Periarticular calcification |
| Hemochromatosis (M>F) | Hands | 2nd and 3rd MCP joint involvement (“squared” metacarpal heads) |
| Alkaptonuria (ochronosis) (M = F) | Intervertebral discs | Degenerative changes: Disc calcification |
| Systemic lupus erythematosus (F>M • affects young adults) | Hands | Reversible MCP joint subluxation |
| Scleroderma (F>M • affects adults) | Hands | IP joint arthritis |
| Mixed connective tissue disease (overlap syndrome) | Hands | PIP joint, MCP joint, mid-carpal involvement |
| Multicentric reticulohistiocytosis (F>M) | Hands and feet | DIP joint and carpal involvement |
| Polymyositis/dermatomyositis | Proximal extremities | Soft tissue calcification |
| Hands | DIP joint erosions | |
| Sarcoidosis | Distal and middle phalanges of the hands and feet | Punched-out cystlike lesions |
| Hemophilic arthropathy (affecting males-but with female carriers) | Predilection for large joints (e.g., knee) | Epiphyseal overgrowth |
| Neuropathic arthropathy | Any joint | 5 “Ds”: Normal bone Density |
| Hypertrophic osteoarthropathy | Tubular bones (radius and ulna >tibia and fibula) | Diaphyseal and metaphyseal painful periostitis |
CPPD, Calcium pyrophosphate deposition disease; DIP, distal interphalangeal; F, female; HA, hydroxyapatite; HLA, human leukocyte antigen; IP, interphalangeal; M, male; MCP, metacarpophalangeal; MTP, metatarsophalangeal; PIP, proximal interphalangeal; Rh, Rhesus; SI, sacroiliac.
From Grant LA, Griffin N: Grainger & Allison’s diagnostic radiology essentials, ed 2, Philadelphia, 2019, Elsevier.
Table 65 Contraindications to Arthrocentesis and Joint Injection
| Contraindication | Comment | ||
|---|---|---|---|
| Established infection in nearby structures (e.g., cellulitis, septic bursitis) | Sometimes gout mimics cellulitis, creating a confusing picture | ||
| Septicemia (theoretic risk of introducing organism into joint) | Need to tap suspected septic joints in septic patients | ||
| Disrupted skin barrier (e.g., psoriasis) | Do not tap through lesions | ||
| Bleeding disorder (not absolute, but use more care) | Risk of bleeding very low, even in patients taking warfarin | ||
| Septic joint | Steroid injection contraindicated | ||
| Prior lack of response | Relative contraindication | ||
| Difficult-to-access joint | Relative contraindication without imaging aid |
From Firestein GS et al: Kelley’s textbook of rheumatology, ed 9, Philadelphia, 2013, Saunders.
Table 66 Synovial Fluid Characteristics in Clinical Situations, with Imaging and Investigation Techniques to Identify the Cause
| Diagnosis | Cells | Microorganisms | Appearance | Imaging Modality | Comments |
|---|---|---|---|---|---|
| Bacterial arthritis | Neutrophils, 10,000->100,000 | Gram stain usually positive | Turbid/pus | May need ultrasound to aspirate dryness | Systemic symptoms, Gram stain, blood and synovial fluid culture |
| Gonococcal arthritis | Neutrophils, 10,000-100,000 | Gram stain usually positive | Turbid/pus | May need ultrasound to aspirate dryness | Systemic symptoms, Gram stain, blood and synovial fluid culture |
| Crystal arthritis | Neutrophils, 10,000->100,000 | - | Turbid/pus | Radiographs, CPPD | Presence of appropriate crystals Acute serum urate unreliable |
| Tuberculous arthritis | Mononuclear 5000-50,000 | Acid-fast stain often negative, may need to culture synovial tissue | Turbid/pus | At-risk population; Ziehl-Neelsen stain biopsy may be necessary | |
| Inflammatory monoarthropathies | Neutrophils 5000-50,000 | - | Slightly turbid | Ultrasound/MRI for early synovitis and erosions | Serum autoantibodies such as RF, ACPA, ANA |
| Osteoarthritis | Mononuclear 0-2000 | - | Clear | Radiographic changes | Usually noninflammatory CPPD may be present |
| Internal derangement | Red blood cells | - | Clear/turbid | MRI | Arthroscopy may be necessary |
| Trauma | Red blood cells | - | Clear/turbid | Radiographs | Tc bone scan may aid diagnosis if radiograph normal |
| Ischemic necrosis | - | MRI in early disease | XR abnormal only in advanced cases | ||
| Uncommon Causes | |||||
| Sarcoidosis | Mononuclear, 5000-20,000 | - | CXR | ||
| PVNS | Red blood cells | - | Turbid | Ultrasound and MRI | Synovial biopsy essential |
| Charcot disease | Mononuclear, 0-2000 | - | Radiographs | CPPD may be present | |
| Lyme disease | Neutrophils, 0-5000 | - | Clear/turbid | SF eosinophilia may be found Serology for Borrelia | |
| Amyloid | Mononuclear, 2000-10,000 | - | Turbid | Synovial biopsy for Congo red stain | |
ACPA, Anticitrullinated protein antibody; ANA, antinuclear antibody; CPPD, calcium pyrophosphate dehydrate deposition; CXR, chest radiograph; PVNS, pigmented villonodular synovitis; RF, rheumatoid factor; SF, synovial fluid; Tc, technetium; XR, radiograph.
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.
Table 67 The Differential Diagnosis of Polyarthritis
| Disease Category | Specific Disease | Mono-, Oligo-, or Polyarthritis (Most Common Presentation) |
|---|---|---|
| Infections | ||
| Viral | Parvovirus B19 | Poly |
| Rubella virus | Poly | |
| Hepatitis A, B, C | Poly | |
| HIV | Oligo, poly | |
| Alphaviruses, including Chikungunya infection | Poly | |
| Bacterial | Gram-positive and gram-negative infections | Mono, occasionally oligo/poly |
| Initial phase of gonorrhea | Poly | |
| Later phase of gonorrhea | Mono | |
| Early phase of Lyme arthritis | Poly | |
| Later phase of Lyme arthritis | Oligo, mono | |
| Diseases Triggered by Infection but Presumed to Be Autoimmune | ||
| Reactive arthritis | After urogenital infections (Chlamydia and Ureaplasma); after gastrointestinal infections (Yersinia, Shigella, Campylobacter, and Salmonella) | Mono, oligo, poly |
| Acute rheumatic fever | After infection with group A streptococcus | Oligo |
| Autoimmune Diseases | ||
| Primary arthritides | Rheumatoid arthritis | Poly |
| Psoriatic arthritis | Oligo, poly | |
| Spondyloarthropathies | Oligo, poly | |
| Juvenile inflammatory arthritis | Mono, oligo, poly | |
| Transient and recurring polyarthritides | Palindromic rheumatism | Poly |
| Recurrent symmetric seronegative synovitis with pitting edema (RS3PE syndrome) | Poly | |
| Systemic autoimmune disease | Systemic lupus erythematosus | Poly |
| Mixed connective tissue disease | Poly | |
| Primary Sjögren syndrome | Poly | |
| Progressive systemic sclerosis and limited scleroderma | Poly | |
| Behçet disease | Oligo, poly | |
| Sarcoidosis | Oligo, poly | |
| Vasculitis | Poly | |
| Autoinflammatory diseases | Adult-onset Still disease | Oligo, poly |
| Familial Mediterranean fever and other cryopyrin-associated fever syndromes | Poly | |
| Various genetic autoinflammatory conditions usually manifested first in childhood | Poly | |
| Degenerative diseases | Includes erosive inflammatory osteoarthritis | Poly |
| Osteoarthritis | ||
| Hypertrophic osteoarthropathy | Poly | |
| Osteonecrosis | Mono, oligo | |
| Metabolic Diseases | ||
| Thyroid diseases | Hypothyroidism | Mono, oligo |
| Hemochromatosis | Hyperthyroidism (Graves disease; early phase of Hashimoto disease) | Oligo, poly |
| Hemoglobinopathies | Sickle cell anemia | Oligo, poly |
| Hemochromatosis | Thalassemia | Oligo, poly |
| Crystal diseases | Gout | Mono (initial), oligo, poly (late stage) |
| Pseudogout | Mono, oligo, poly | |
| Deposition diseases | Glycogen storage diseases; amyloid deposition in primary amyloidosis; mucopolysaccharidoses; light- and heavy-chain deposition diseases; others | Oligo, poly |
| Drug-Induced Diseases | ||
| Vasculitic drug reactions, serum sickness | Poly | |
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.