AUTHORS: Hesham Shaban, MD and Junior Uduman, MD
Rhabdomyolysis is a syndrome characterized by striated muscle lysis with resulting muscle damage and leakage of intracellular contents into the circulation. The presentation may range from an asymptomatic elevation of creatine kinase (CK) to severe muscle injury with irreversible kidney failure. In general, a 5- to 10-fold elevation of CK levels, muscle pain, and myoglobinuria in an appropriate clinical setting (see below) are sufficient criteria for the diagnosis of rhabdomyolysis. Acute kidney injury (AKI), which is not a diagnostic criterion of rhabdomyolysis, typically results from multiple factors, including volume depletion, tubular obstruction, direct heme pigment-induced proximal tubular cell injury, and renal vasoconstriction.
| ||||||||||||||||
- Evidence is limited regarding the onset of physical exertion-induced rhabdomyolysis. Exercise levels that exceed an individual’s usual exercise tolerance level commonly induce rhabdomyolysis. Extracellular volume depletion and vasoconstriction are common predisposing features. Patients with risk factors (e.g., metabolic myopathies, advanced age) develop symptoms associated with rhabdomyolysis within 2 to 6 hr after activity. Concurrent electrolyte abnormalities such as hypokalemia, hyponatremia, hypernatremia, hypomagnesemia, hypophosphatemia, and hypocalcemia increase the risk for rhabdomyolysis. Patients without risk factors generally become symptomatic 12 to 36 hr after muscle injury.
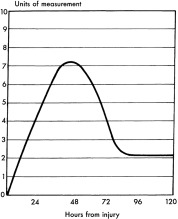
- CK levels increase within 2 to 12 hr of the onset of muscle injury, generally peak after 24 to 72 hr, and decline 3 to 5 days after cessation of muscle injury. Peak CK levels may predict development of AKI.
- Rhabdomyolysis from cholesterol-lowering therapy by HMG-CoA reductase inhibitors (statins) requires hospitalization in less than 0.1% of cases. The mechanism of damage is multifactorial: Bioavailability, lipophilicity, efficiency of uptake of transport proteins in hepatocytes, blood level of statins, and level of extrahepatic inhibition of mitochondrial respiration, bioavailability, and lipophilicity. Among the statins, pravastatin has a lower risk for induction of rhabdomyolysis than other statins, presumably due to lower lipid solubility. The average duration of statin therapy before onset of myopathy is 6 mo. Symptom resolution with normalization of serum CK concentrations occurs in days to weeks following drug discontinuation. The average time for onset of rhabdomyolysis after the addition of a fibrate to statin therapy is 32 days. Rare genetic variants are associated with statin-induced myopathy.
- Classic triad of muscle pain, weakness, and dark urine from myoglobinuria
- Muscle tenderness is present in half of cases
- Muscle swelling occurs after intravenous fluid repletion
- Muscular rigidity
- Fever
- In rhabdomyolysis secondary to long-term statin administration, fatigue (74%) is nearly as common as muscle pain (88%)
- Oliguria or anuria with AKI
Causes can be divided into three categories:
- Traumatic or muscle compression
- Nontraumatic exertional
- Exercise: More than 10 genetically predisposing gene sequence variants are associated with exertional rhabdomyolysis
- Sickle cell trait, rarely: Usually additional predisposing factors are involved (e.g., body mass index [BMI] >30 kg/m2, tobacco use, statin use, antipsychotic use, high altitude)
- Heat stroke
- Metabolic myopathies
- Malignant hyperthermia and neuroleptic malignant syndrome
- Seizure activity
- Nontraumatic, nonexertional
- Drug-induced (statins alone, combinations of statins with fibrates or erythromycin, simvastatin and amiodarone, amphetamines, haloperidol, levofloxacin, macrolide antibiotics)
- Chronic ethanol ingestion
- Hypothyroidism
- Infectious and inflammatory myositis
Table 1 summarizes various causes of rhabdomyolysis.
TABLE 1 Causes of Rhabdomyolysis
| Muscle injury/ischemia | Trauma, pressure necrosis, electric shock, burns, acute vascular disease | ||
| Myofiber exhaustion | Seizures, excessive exercise, heat exhaustion | ||
| Toxins | Alcohol, cocaine, heroin, amphetamines, ecstasy, phencyclidine, snakebite | ||
| Drugs | Statins, fibrates, zidovudine, neuroleptic malignant syndrome, azathioprine, theophylline, lithium, diuretics, colchicine | ||
| Electrolyte disorders | Hypophosphatemia, hypokalemia, excess water shifts (hyperosmolality) | ||
| Infections | Viral (influenza, HIV, coxsackievirus, Epstein-Barr virus), bacterial (Legionella, Francisella, Streptococcus pneumoniae, Salmonella, Staphylococcus aureus) | ||
| Familial | McArdle disease, carnitine palmitoyl transferase deficiency, malignant hyperthermia | ||
| Other | Hypothyroidism, polymyositis, dermatomyositis |
From Floege J et al: Comprehensive clinical nephrology, ed 4, Philadelphia, 2010, Saunders.