AUTHORS: Kenny Chang, BS and Manuel F. DaSilva, MD
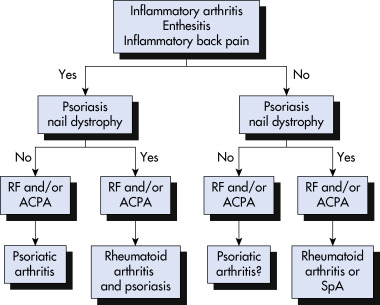
Psoriatic arthritis (PsA) is an inflammatory arthropathy, often included in a class of disorders called the seronegative spondyloarthropathies (SpA), a family of diseases characterized by inflammation of the spine, peripheral joints, and entheses (sites of insertion of tendon into bone).1 Both the Moll and Wright and CASPAR classification criteria are described in Table 1.
| ||||||||||||||||
TABLE 1 Classifications of Psoriatic Arthritis
| Moll and Wright | CASPAR∗ | ||
|---|---|---|---|
| Points | Category | Description | |
| Presence of PsO and an inflammatory arthritis (peripheral arthritis and/or sacroiliitis or spondylitis) The (usual) absence of serologic tests for RF | 2 | Current PsO | Psoriatic skin or scalp disease confirmed by a dermatologist or rheumatologist; history of PsO from the patient, family physician, dermatologist, rheumatologist, or other qualified practitioner; patient-reported history of PsO in a first- or second-degree relative |
| 1 | Personal or family history of PsO | ||
| 1 | Psoriatic nail dystrophy on current physical examination | Includes onycholysis, pitting, and hyperkeratosis | |
| 1 | Negative test for RF | ELISA or nephelometry preferred (no latex) using the local laboratory reference range | |
| 1 | Current dactylitis or history of dactylitis documented by a rheumatologist | Swelling of the entire digit | |
| 1 | Radiographic evidence of juxtaarticular new bone formation | Ill-defined ossification near joint margins in the hand or foot, excluding osteophyte formation on plain radiographs | |
CASPAR, Classification Criteria for the Study of Psoriatic Arthritis; ELISA, enzyme-linked immunosorbent assay; PsO, psoriasis; RF, rheumatoid factor.
∗Psoriatic arthritis is diagnosed when three or more points are assigned in the presence of inflammatory articular disease (joint, spine, or entheseal).
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
One to two per 1000 in the general population.3 Variable estimates of 4% to 30% of patients with underlying psoriasis3
Symptom onset generally between age 30 to 55, although it can begin during childhood4
- Psoriasis precedes arthritis in 67% of cases by an average of 8 to 10 years.5
- Arthritis precedes psoriasis or occurs concomitantly in 33% of patients.5
- Arthritis, dactylitis, spondylitis, and enthesitis are the main features.6
- Arthritis is inflammatory and commonly characterized by prolonged morning stiffness, improvement with activity, joint erythema, warmth, or swelling.3
- There are five classically described patterns of joint involvement (Box 1).
- Some patients may present with more than one pattern, which can evolve over time.3 The distal interphalangeal (DIP) joints (Fig. E1) and spine are each affected in 40% to 50% of cases. It is rare to have spondyloarthritis alone, and it usually occurs with peripheral involvement.3
- Dactylitis, also known as “sausage digit,” refers to diffuse swelling of a finger or toe (Fig. E2); it is fairly common and occurs in approximately 30% to 40% of patients during the disease course.7 It is associated with increased risk of radiographic joint damage.7
- Enthesitis commonly occurs at the Achilles tendon and plantar fascia (Fig. E3), and swelling and tenderness may be seen upon exam.6 Subclinical disease may be evident by ultrasonography.3
- Dystrophic changes of the nails (pitting, onycholysis, and leukonychia) may occur in association with joint inflammation in involved digits.6
- Spondyloarthritis may include sacroiliitis but is generally less likely to cause fusion to the extent seen in ankylosing spondylitis.3 It is more common to have asymmetric sacroiliac joint involvement (usually bilateral in ankylosing spondylitis).3
- Ocular inflammation including conjunctivitis and uveitis can be seen.7
BOX 1 Subtypes of Psoriatic Arthritis
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
Figure E1 Symmetric polyarthritis resembling rheumatoid arthritis.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
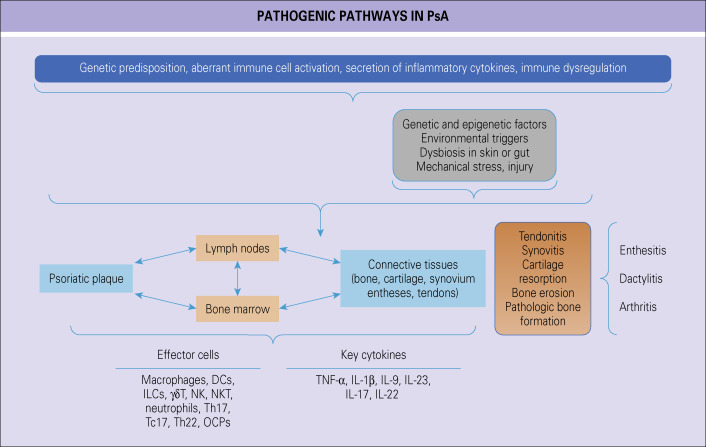
Experts theorize the cause of PsA to be an interplay of genetic, immunologic, and environmental factors. Fig. 4 illustrates the pathogenetic pathways in PsA. There is a higher frequency of HLA-B12, HLA-B17, HLA-B57, HLA-Cw∗0602 in PsA. Those with PsA versus psoriasis alone have higher frequency of HLA-B27.6
In a Subset of Patients with Psoriasis, Epigenetic and Environmental Events in Patients with Specific Genetic Risk Variants Result in Musculoskeletal Inflammation in an Array of Connective Tissues. Effector Cells Release Cytokines that Promote Inflammation in Tendon-Ligament-Synovial Capsule Insertion Sites, Tendons, Synovium, and Bone. This is Accompanied by Bone and Cartilage Damage and Pathologic New Bone Formation. The Resulting Clinical Phenotypes Manifest as Enthesitis, Synovitis, and Dactylitis. Dc, Dendritic Cell; Il, Interleukin; Ilc, Innate Lymphocyte; Nk, Natural Killer; Ocp, Osteoclast Precursors; Psa, Psoriatic Arthritis; Tc17, Cd8+ Il-17 Secreting Cell; Th17, Cd4+ Il-17 Secreting Cell; Th22, Il-22 Secreting Cd4+ Cell; Tnf, Tumor Necrosis Factor.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2019, Elsevier.
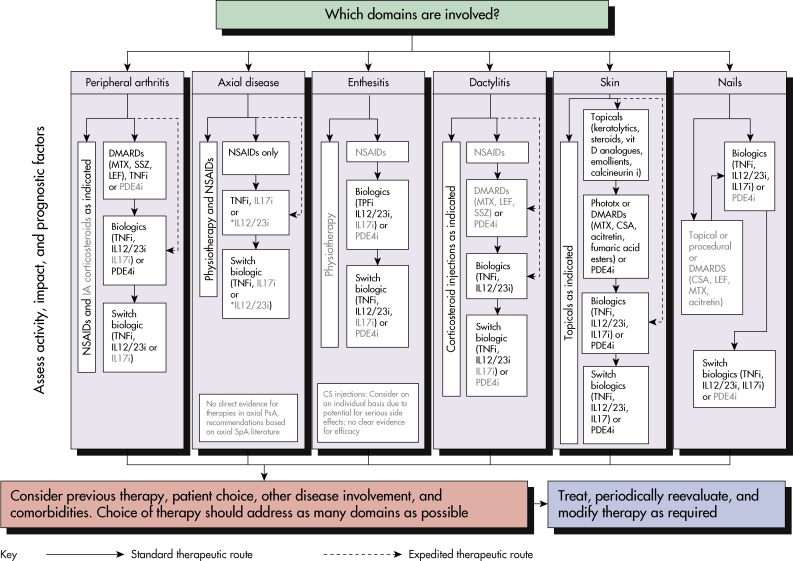
Light Text Identifies Conditional Recommendations for Drugs that Do Not Currently have Regulatory Approvals or for Which Recommendations are Based on Abstract Data Only. CS, Corticosteroid; Csa, Cyclosporine A; Dmards, Disease-Modifying Antirheumatic Drugs; IA, Intraarticular; Il12/23i, Iinterleukin-12/23 Inhibitor; Lef, Leflunomide; Mtx, Methotrexate; NSAIDs, Nonsteroidal Antiinflammatory Drugs; PDE-4i, Phosphodiesterase 4 Inhibitor (Apremilast); Phototx, Phototherapy; Spa, Spondyloarthritis; Ssz, Sulfasalazine; Tnfi, Tumor Necrosis Factor Inhibitor; Vit, Vitamin.
From Firestein GS et al: Firestein & Kelly’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.