AUTHOR: Glenn G. Fort, MD, MPH

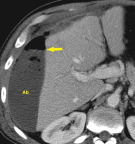
DefinitionA localized accumulation of infected fluid, often encapsulated, located under the diaphragm and may also involve the liver and spleen
SynonymsSubdiaphragmatic abscess
Infradiaphragmatic abscess
| ICD-10CM CODES | | K65.1 | Peritoneal abscess | | K68.11 | Postprocedural retroperitoneal abscess |
|
Epidemiology & DemographicsIncidenceNot well known but intraabdominal abscess occurs in 1% to 2% of all cases of abdominal surgery. It increases to 10% to 30% in cases with preoperative perforation of a hollow viscus, spillage of fecal material into peritoneum, or intestinal ischemia.
Risk Factors
- Abdominal surgery, especially with accidental viscus perforation
- Peptic ulcer perforation
- Appendiceal perforation
- Diverticulitis with perforation
- Mesenteric ischemia with bowel infarction
- Abdominal trauma especially penetrating trauma
- Foreign body ingestion with subsequent viscus perforation
Physical Findings & Clinical Presentation
- Constitutional symptoms include:
- Fever, malaise, or chills
- Cough, increased respiratory rate with shallow or grunting respiration
- Shoulder-tip pain on affected side (referred pain)
- Physical findings can include:
- Dullness to percussion on affected side
- Diminished or absent breath sounds on affected side
- Tenderness over the eighth to eleventh ribs
EtiologyInfection is usually polymicrobial: Aerobic gram-negative rods, most commonly Escherichia coli, Klebsiella species, Enterobacter species, and Pseudomonas aeruginosa, and gram-positive cocci: Streptococcus viridans, enterococci, and Staphylococcus aureus, and anaerobes (found in 60% to 70% of cases) such as Bacteroides fragilis and Clostridia species.

Includes source control with either percutaneous drainage or surgery and intravenous antibiotics:
- Percutaneous drainage via interventional radiology:
- Percutaneous drainage1 with catheter placement remains the preferred treatment despite the fact that the subphrenic location can be problematic for imaging-guided percutaneous drainage.
- Approaches include subcostal approach or intercostal approach. The intercostal approach is associated with a higher risk for pleural complications, but these tend to be minor.2
- Radiographic modalities used include ultrasonography, CT, and fluoroscopy.
- Complications of drainage procedures can include pleural effusion, pneumothorax, or empyema.
- Surgery: May be required in recurrence of abscess or due to multiple abscesses not amenable to percutaneous drainage procedure
- Antibiotics: Broad-spectrum antibiotics should be used to cover gram-negative rods, gram-positive bacteria, and anaerobes until cultures are resulted and should be continued at least 4 to 7 days after adequate drainage procedure. Examples include:
- Piperacillin/tazobactam 3.375 g IV q6h or 4.5 g IV q8h
- Meropenem 1 g IV q8h or imipenem 0.5 to 1 g IV q6h
- Ciprofloxacin IV 400 mg IV q12h plus IV metronidazole 500 mg IV q8h for penicillin allergic patients
Referral
- Interventional radiology
- General surgery
- Infectious diseases