AUTHOR: Glenn G. Fort, MD, MPH



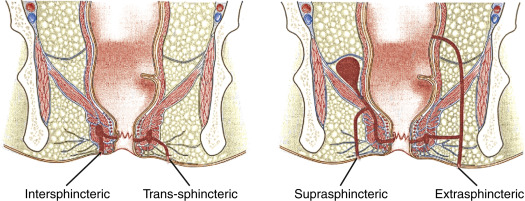
DefinitionA perirectal abscess is a localized inflammatory process that can be associated with infections of soft tissue and anal glands based on anatomic location. Perianal and perirectal abscesses may be simple or complex, causing suppuration. Infections in these spaces may be classified as superficial perianal or perirectal with involvement in the following anatomic spaces: Ischiorectal, intersphincteric, perianal, and supralevator. The Parks classification of anorectal abscess is subdivided into intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric abscess (Fig. 1).
Figure 1 Parks classification of anorectal abscess.
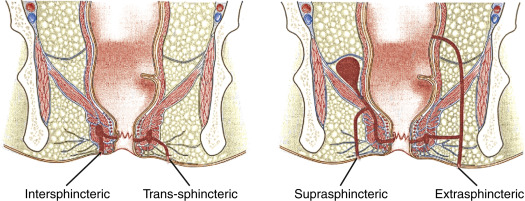
From Cameron JL, Cameron AM: Current surgical therapy, ed 10, Philadelphia, 2011, Saunders.
SynonymsRectal abscess
Perianal abscess
Anorectal abscess
| ICD-10CM CODES | | K61.0 | Anal abscess | | K61.1 | Rectal abscess |
|
Epidemiology & DemographicsIncidence (In U.S.)Commonly encountered
Predominant SexMale >female
Peak IncidenceNot seasonal; common
Physical Findings & Clinical Presentation
- Localized perirectal or anal pain-often worsened with movement or straining
- Perirectal erythema or cellulitis
- Perirectal mass by inspection or palpation
- Fever and signs of sepsis with deep abscess
- Urinary retention
Etiology
- Polymicrobial aerobic and anaerobic bacteria involving one of the anatomic spaces (see “Definition”), often associated with localized trauma
- Microbiology: Most infections are polymicrobial, mixed enteric, and skin flora
- Predominant anaerobic bacteria:
- Bacteroides fragilis
- Peptostreptococcus spp.
- Prevotella spp.
- Porphyromonas spp.
- Clostridioides spp.
- Fusobacterium spp.
- Predominant aerobic bacteria:
- Staphylococcus aureus
- Streptococcus spp.
- Escherichia coli
- Enterococcus spp.

Many patients will have predisposing underlying conditions including:
- Malignancy or leukemia
- Immune deficiency
- Diabetes mellitus
- Recent surgery
- Steroid therapy
Differential Diagnosis
- Neutropenic enterocolitis
- Crohn disease (inflammatory bowel disease)
- Pilonidal disease
- Hidradenitis suppurativa
- Tuberculosis or actinomycosis; Chagas disease
- Cancerous lesions
- Chronic anal fistula
- Rectovaginal fistula
- Proctitis-often STD-associated, including syphilis, gonococcal, chlamydia, chancroid, condylomata acuminata
- AIDS-associated: Kaposi sarcoma, lymphoma, cytomegalovirus
Workup
- Examination of rectal, perirectal/perineal areas
- Rule out necrotic process and crepitance suggesting deep tissue involvement
- Local aerobic and anaerobic culture
- Blood cultures if toxic, febrile, or compromised
- Possible sigmoidoscopy
Imaging StudiesUsually not indicated unless extensive disease is suspected. CT has a sensitivity of 77% and is relatively poor in detecting a perirectal abscess in immunocompromised patients.

Perirectal abscess may be a presenting manifestation of type 2 diabetes mellitus in older adults. Check the blood sugar in patients to exclude the possibility of undiagnosed diabetes mellitus.
Related ContentPerirectal Abscess (Patient Information)