AUTHOR: Glenn G. Fort, MD, MPH
Necrotizing fasciitis (NF) is a rapidly spreading bacterial infection of the deep fascia, with associated inflammation, leading to necrosis of subcutaneous tissue planes. This infection can occur in wounds from trauma or surgical wounds or can be spontaneous or idiopathic. There are two clinical types, both of which carry a high rate of morbidity and mortality.
- Type I: Necrotizing fasciitis: At least one anaerobic species is isolated in conjunction with one or more facultative anaerobic species, such as streptococci (not group A), and members of the Enterobacteriaceae (gram-negative rods)
- Anaerobic bacteria, most commonly Bacteroides or Peptostreptococcus spp.
- Enterobacteriaceae: Escherichia coli, Klebsiella spp., Proteus spp., Enterobacter spp.
- Usually associated with diabetes or peripheral vascular disease
- Example of type I: Fournier gangrene of the perineum
- Type II: Necrotizing fasciitis: Group A Streptococcus is isolated alone or in combination with other bacteria, most likely Staphylococcus aureus. Also known as hemolytic streptococcal gangrene
- Fournier gangrene: Aggressive type I infection of the perineum usually caused by penetration of the gastrointestinal or urethral mucosa by enteric organisms. It can rapidly spread to involve the scrotum, penis, and abdominal wall or gluteal muscles, causing gangrene. Use of sodium-glucose cotransporter-2 (SGLT2) inhibitors in diabetics has been associated with Fournier gangrene.
- Clostridial cellulitis: Caused by Clostridium perfringens associated with local trauma or surgery and crepitus caused by gas production; generally noted in the skin, with deeper tissues generally spared.
Minor skin trauma, toxic-appearing patient:
- Open skin wound
- Severe pain at injury or surgical site
- Fever, confusion, weakness, diarrhea
- Early skin erythema, quickly spreading in hours to days
- Skin redness changes to purple discoloration
- Gangrenous skin changes may develop
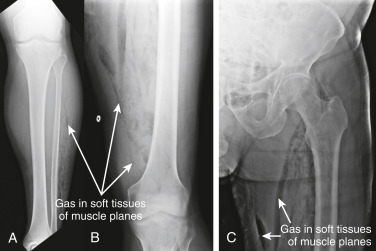
- Loosening of skin and subcutaneous skin in association with deep fascial necrosis (Fig. E1). “Woody” induration and crepitus of involved area are characteristics
- Muscle involvement, thrombosis of blood vessels, and myonecrosis may develop
- Bullae and gas formation at site
Figure E1 Necrotizing fasciitis.
The so-called flesh-eating bacteria, group A β-hemolytic Streptococcus, can cause significant tissue destruction rapidly. This 32-yr-old woman had pain, erythema, and swelling of the foot followed by necrotic ulceration over a week. There was no history of trauma.
Courtesy Roger Bitar, MD. From White GM, Cox NH [eds]: Diseases of the skin, a color atlas and text, ed 2, St Louis, 2006, Mosby.
- NF usually arises from skin damage or trauma. Risk is increased with presence of comorbidities (diabetes mellitus, cancer, liver disease, immunosuppression, use of SGLT2 inhibitors)
- Polymicrobial: Mixture of anaerobes and aerobic enteric gram-negative rods
- Group A streptococci (S. pyogenes)
- S. aureus
- C. perfringens
- Bacteroides fragilis
- Vibrio vulnificus
- Methicillin-resistant S. aureus (MRSA), especially community-acquired MRSA