AUTHORS: Benjamin J. Ahn, BS and John D. Milner, MD, and Manuel F. DaSilva, MD
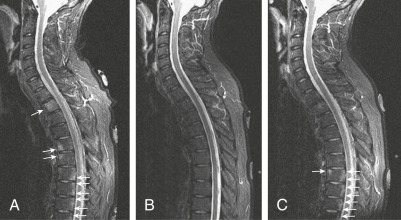
Ankylosing spondylitis (AS) is a type of inflammatory arthritis involving the sacroiliac joints and axial skeleton characterized by ankylosis (abnormal stiffening of a joint) and enthesitis (inflammation at tendon insertions). It is part of a family of overlapping syndromes called seronegative spondyloarthropathies (SpA) that includes reactive arthritis (formerly Reiter syndrome), psoriatic spondylitis, and enteropathic arthritis.1
| ||||||||||||||||||||||||||||||||||||||||||||||||
Between 0.1% and 1% of the population. Varies with prevalence of HLA-B27 and ethnicity. The U.S. prevalence of AS has been reported between 5% and 6% in HLA-B27 populations. Much higher in those with positive family history of spondyloarthropathy.2
- Prolonged morning back stiffness of insidious onset lasting more than 3 mo
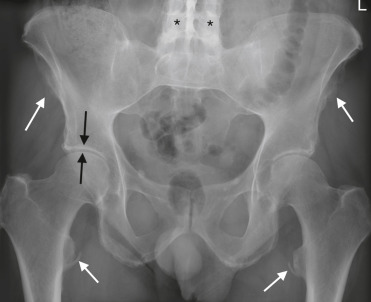
- Bilateral sacroiliac joint tenderness (sacroiliitis)
- Inflammatory back pain; often improves with exercise and is worse with rest
- Limited lumbar spine motion
- Tenderness at tendon insertion sites, especially the Achilles tendons and plantar fascia
- Loss of chest expansion reflecting rib cage involvement
- Possible to have peripheral joint arthritis, usually involving lower extremities
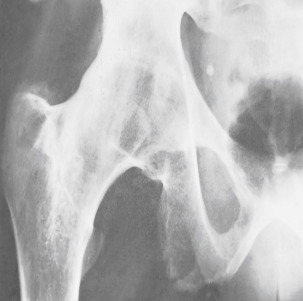
- In advanced cases the typical posture consists of compensatory hyperextension of neck, fixed flexion of hips, and compensatory flexion of knees (Fig. 1)
- There is an increased incidence of iritis and uveitis (30% to 40% lifetime prevalence)
- Other extra-skeletal manifestations include effects on the cardiovascular system (aortic insufficiency, cardiovascular disease), cerebrovascular system, and lungs (pulmonary fibrosis). There is also an increased risk for osteoporosis.3,4
From Talley NJ et al: Essentials of internal medicine, ed 4, Chatswood, NSW, 2021, Elsevier Australia.
TABLE E1 Aspects of Inflammatory Back Pain in Ankylosing Spondylitis and Axial Spondyloarthritis
| Onset of symptoms before age 45 yr | |||
| Duration of symptoms more than 3 mo (chronic pain) | |||
| Located at the lower back | |||
| Alternating buttock pain | |||
| Awaking due to back pain during the second half of the night | |||
| Morning stiffness for at least 30 min | |||
| Insidious onset of complaints | |||
| Improvement with exercises | |||
| No improvement of back pain with rest | |||
| Improvement with use of nonsteroidal agents |
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.
TABLE E2 Characteristic Features of Ankylosing Spondylitis
| Chronic inflammatory spinal pain | |||
| Chest pain | |||
| Alternate buttock pain | |||
| Acute anterior uveitis | |||
| Synovitis (predominantly of lower limbs, asymmetric) | |||
| Enthesitis (heel, plantar) | |||
| Radiographic sacroiliitis | |||
| Positive family history of ankylosing spondylitis | |||
| Chronic inflammatory bowel disease | |||
| Psoriasis |
From Firestein GS et al: Firestein & Kelley’s textbook of rheumatology, ed 11, Philadelphia, 2021, Elsevier.
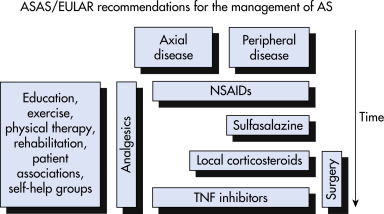
Although significant progress has been made, the etiology of AS still remains unclear to an extent. To date, it is believed that genetic background, immune reactions, infection, and endocrinal abnormities play a role in susceptibility to the spondyloarthropathies. Major histocompatibility complex class I allele HLA-B27 has been described as the predominant genetic predisposing factor. Infections such as Klebsiella pneumonia, an opportunistic pathogen that makes up part of the normal gut microflora, may be an exacerbating agent in the autoimmune process of AS. Tumor necrosis factor is important in the inflammatory response.5