AUTHOR: Glenn G. Fort, MD, MPH
Infection with cytomegalovirus (CMV), a herpes virus, is common in the general population, with multiple mechanisms for transmission, often during childhood and adolescence. CMV is associated with pregnancy and can be a congenital disease. CMV is also associated with immunocompromised states and may be life-threatening.
Heterophil-negative mononucleosis
Cytomegalic inclusion disease virus
| ||||||||||||||||
Congenital-25% of infected children with symptoms if congenital:
- Petechial rash
- Jaundice and/or hepatosplenomegaly
- Lethargy
- Respiratory distress
- Central nervous system (CNS) involvement, seizures
- CMV mononucleosis
- Pharyngitis, croup, bronchitis, pneumonia
- May be asymptomatic
- CMV mononucleosis similar to Epstein-Barr virus (EBV) mononucleosis
- Fever-lasting 9 to 30 days-mean of 19 days
- Exudative pharyngitis
- Lymphadenopathy, hepatitis, splenomegaly
- Interstitial pneumonia (rare)
- Nonspecific rash
- Thrombocytopenia/hemolytic anemia
- Febrile mononucleosis
- GI ulcerations, hepatitis, pneumonitis, retinitis, encephalopathy, meningoencephalopathy
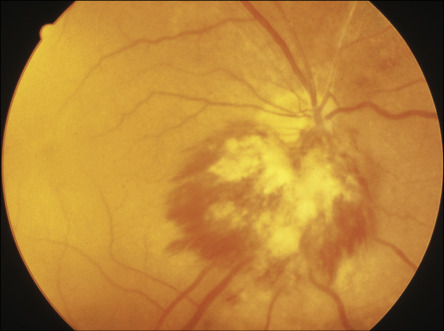
- HIV associated-dementia, demyelination, retinitis (Fig. E1), acalculous cholecystitis, adrenalitis, diarrhea, enterocolitis, esophagitis
- Diabetes associated with pancreatitis
- Adrenalitis associated with HIV