Differential Diagnosis
- Primary hyperparathyroidism:
- Adenoma (80%)
- Hyperplasia (15% to 20%)
- Carcinomas (<1%)
- Secondary hyperparathyroidism (Box 1) precipitated by conditions that result in hypocalcemia:
- Renal calcium loss (i.e., medication: Loop diuretics and hypercalciuria)
- Calcium deficiency
- Vitamin D deficiency
- Malabsorption
- Chronic kidney disease (most common)2
- Pseudohypoparathyroidism (PTH resistance)
- Inhibition of bone resorption (i.e., bisphosphonates and denosumab)
- Other causes of hypercalcemia (Table 2) include:
- Medications: Thiazide diuretics, lithium therapy
- Vitamin D intoxication, milk-alkali syndrome
- Vitamin A toxicity
- Familial hypocalciuric hypercalcemia (FHH)
- Renal failure (tertiary hyperparathyroidism)
- Thyrotoxicosis
- Granulomatous disorders (e.g., sarcoidosis)
- Malignancy (e.g., lung cancer, lymphoma, multiple myeloma, and bone metastasis)
- Prolonged immobilization
TABLE 2 Causes of Hypercalcemia
| Endocrine | Primary hyperparathyroidism |
| Tertiary hyperparathyroidism |
| Familial hypocalciuric hypercalcemia |
| Hyperthyroidism |
| Malignancy | Tumors producing PTHrP (SCC of lung, bladder cancer, renal cell cancer) |
| Osteolytic bone metastasis |
| Hematologic malignancies (lymphoma, leukemia, multiple myeloma) |
| Granulomatous disease | Sarcoidosis |
| Tuberculosis |
| Fungal infection |
| Medications | Calcium |
| Thiazide diuretics |
| Lithium |
| Vitamin A and D intoxication |
| Milk alkali syndrome |
| Miscellaneous | Paget and other bone diseases with prolonged immobilization |
PTHrP, Parathyroid hormone-related peptide; SCC, squamous cell carcinoma.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
BOX 1 Causes of Secondary Hyperparathyroidism
- Chronic renal failure
- 25-Hydroxyvitamin D deficiency
- Malabsorption syndromes
- Celiac disease
- Cystic fibrosis
- Short gut syndrome
- Bariatric procedures
- Medications
- Metabolic abnormalities
- Hypermagnesemia
- Hyperphosphatemia
- Congenital disorders
- Transient neonatal hyperparathyroidism
- DiGeorge syndrome
|
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
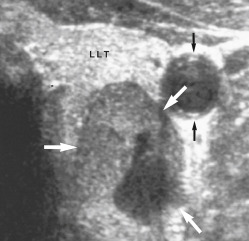
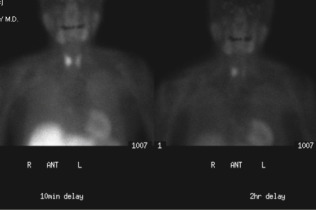
Imaging Studies (Table 4
- Parathyroid localization with technetium-99m sestamibi (Fig. E2 and Fig E3) can identify potential adenomas to help with surgical planning.8 The inferior parathyroid glands are more commonly ectopic and can be found anywhere from the angle of the mandible to the pericardium. The most common ectopic location for an inferior gland is within the thymus (Fig. 4)
- Parathyroid ultrasound (Fig. 5, Fig E6), dynamic (4D) CT, and MRI are also used to localize the parathyroid adenoma.8
- Bone mineral density (BMD) imaging of the spine, hip, and forearm (distal third of radius) is recommended for all patients with hyperparathyroidism to assess the risk for osteoporosis and fragility fractures. Plain radiographic abnormalities are illustrated in Fig. E7 and Fig. E8. Cortical bone loss (i.e., distal one third radius) is greater than trabecular bone loss (i.e., hip and spine) in hyperparathyroidism.9
- Renal ultrasound can be considered to assess asymptomatic renal stones.
Figure 5 High-Resolution Ultrasonography of the Left Lobe of the Thyroid (Llt) Anterior to a Parathyroid Adenoma (White Arrows)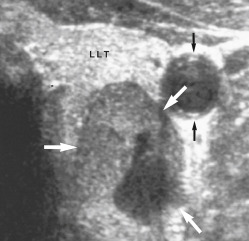
There is a small area of cystic degeneration within the posterior aspect of the adenoma. Carotid artery (black arrows).
From Adam A et al: Grainger & Allison’s diagnostic radiology, ed 5, London, 2007, Churchill Livingstone. In Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, London, 2019, Elsevier.
TABLE 4 Characteristics of Preoperative Imaging Studies in Patients With Hyperparathyroidism
| Imaging | Imaging Findings | Sensitivity, Ppv | Advantages | Limitations | Updates |
|---|
| US | Hypoechoic nodule with well-defined hypervascular echogenic capsule | 76%, 93% | Noninvasive, inexpensive, can be performed rapidly by the surgeon with simultaneous evaluation of the thyroid | Unable to see ectopic mediastinal, retroesophageal, or retropharyngeal glands; decreased sensitivity in multigland disease and small glands; thyroid nodules and lymph nodes can cause false-positives | US elastography |
| Sestamibi-SPECT | Increased focal uptake and prolonged retention of the technetium-99m sestamibi | 79%, 90% | Detects ectopic and posterior glands; lower radiation than 4D-CT, operator-independent | Long duration of time for the exam; more expensive than US and 4D-CT, radiation exposure; decreased sensitivity for multigland disease and small glands; false-positives (lymph nodes, thyroid tissue, granulomatous disease) | PET scanning with various radiopharmaceuticals under investigation |
| 4D-CT | Soft tissue nodule with peaked enhancement in arterial phase and washout in venous phase with polar vessel | 81%-89%, 93% | Rapid acquisition time, superior anatomic information, superior sensitivity than other techniques, more successful in localizing small adenomas and multigland disease | High radiation dose, intravenous contrast use, some contrast artifact in neck veins can occur | Protocols with fewer phases or less contrast, to diminish radiation and contrast dose |
| MRI | Homogeneous or marbled appearance with high intensity on T2-weighted images, intermediate to low intensity on T1-weighted images | 43%-94% | No radiation, contrast not necessary, superior anatomic information | Expensive, long duration of study acquisition, cannot use in patients with metal implants, low specificity | Dixon fat suppression method |
| 18F-fluorocholine PET/CT | Focal tracer uptake | 93%, 90% | Decreased radiation and acquisition time compared to some sestamibi protocols, higher sensitivity | Limited data on new tracer, limited availability | Ability to differentiate between parathyroid adenoma and hyperplasia preoperatively based on maximal standardized uptake values |
CT, Computed tomography; 4D-CT, four-dimensional CT; MRI, magnetic resonance imaging; PET/CT, positron emission tomography/CT; SPECT, single photon emission CT; US, ultrasound.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Figure E2 Role of scintigraphy in detecting parathyroid adenomas.
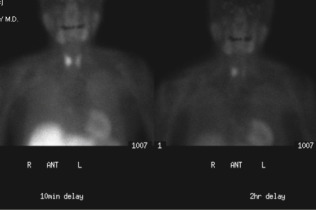
A 66-yr-old woman with hypercalcemia. CT (not shown) did not reveal a parathyroid adenoma. 99mTc-sestamibi radionuclide imaging demonstrates uptake in both thyroid and parathyroid parenchyma in the 10-min delayed image (left); however, at 2-h delay, imaging (right) demonstrates persistent uptake in the right lobe of the thyroid gland, representing the parathyroid adenoma.
From Adam A et al: Grainger and Allison’s diagnostic radiology, ed 6, London, 2015, Elsevier. In Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, London, 2019, Elsevier.
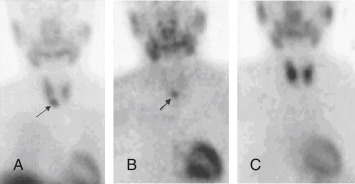
Figure E3 Ectopic intrathymic parathyroid adenoma.

From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Figure E4 Parathyroid adenoma.
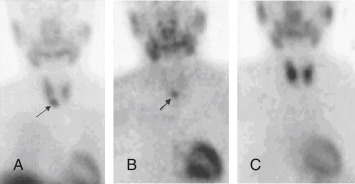
99mTc-MIBI images at 10 min (A) and 3 h (B), showing a persistent focus of activity inferior to the right lobe of the thyroid; 99mTcO 4 image (C) shows normal thyroid uptake but the adenoma is not visualized.
From Grant LA et al: Grainger & Allison’s diagnostic radiology essentials, ed 2, Philadelphia, 2019, Elsevier.
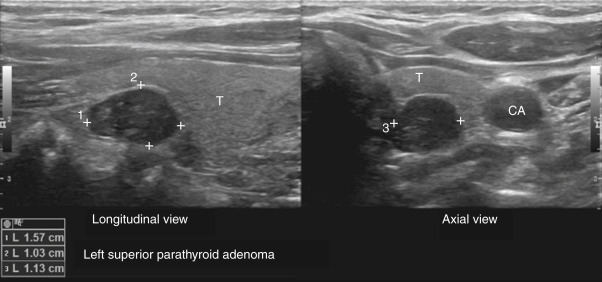
Figure E6 High-Resolution Ultrasound Images Demonstrating a 157 × 1.03 × 1.13 cm Hypoechoic Mass Posterior to the Superior Pole of the Left Lobe of the Thyroid Gland in Longitudinal and Axial Views, Which Corresponded to a Left Superior Parathyroid Adenoma.
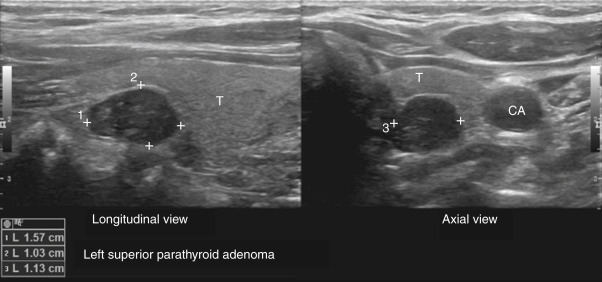
Parathyroid gland marked by measuring points. CA, Carotid artery; T, thyroid.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Figure E7 Hyperparathyroidism.

Chondrocalcinosis in the knee menisci (A) and (B) the symphysis pubis. (C) Subperiosteal erosions along the radial side of the middle phalanx of the 2nd finger. Acroosteolysis is also present. Metastatic calcification of the digital artery confirms this is secondary hyperparathyroidism. (D) Cortical “tunneling” in the proximal phalanges. (E) Brown tumor within the distal tibia. (F) Precipitation of amorphous calcium phosphate in the soft tissues of the shoulder (hyperparathyroidism secondary to chronic renal disease).
From Adam A et al: Grainger & Allison’s diagnostic radiology, ed 5, London, 2007, Churchill Livingstone. In Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, London, 2019, Elsevier.
Figure E8 Secondary hyperparathyroidism.

Lateral radiograph of the thoracic spine demonstrating increased sclerosis along the end plates and increased lucency of the central part, giving a “rugger jersey” spine appearance. Also note deformity of the vertebral bodies, with loss of height and increased diameter, in addition to wedge-shaped deformities at the upper thoracic spine related to decreased stability and weakness of the abnormal bone.
From Adam A et al: Grainger and Allison’s diagnostic radiology, ed 6, London, 2015, Elsevier. In Grant LA: Grainger & Allison’s diagnostic radiology essentials, ed 2, London, 2019, Elsevier.