AUTHOR: Ali Ahmad, MD
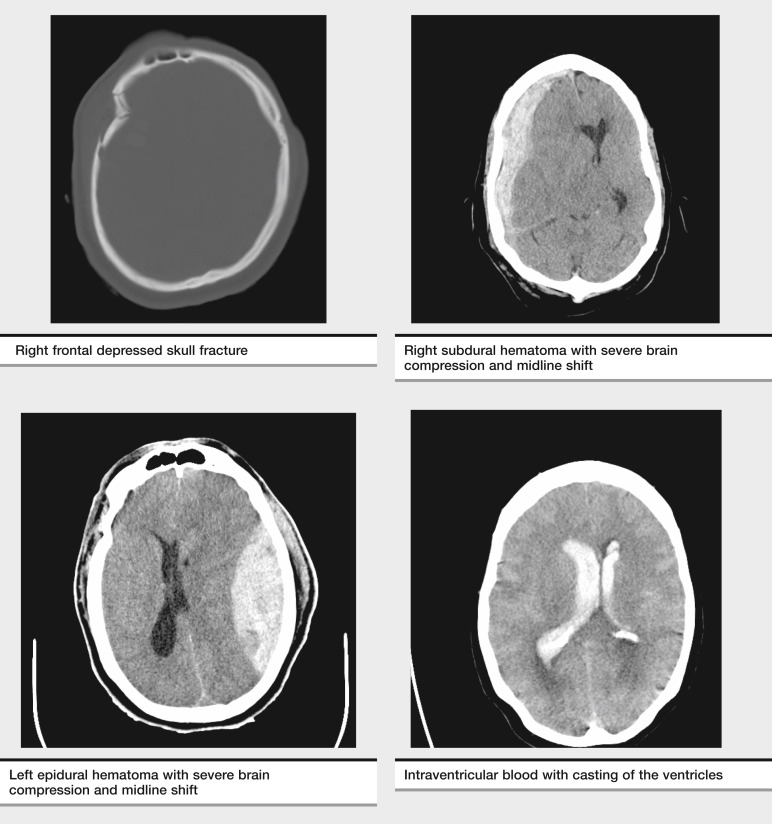
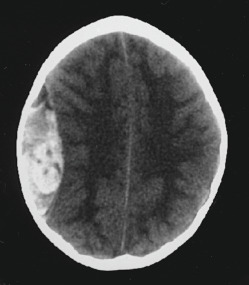
- Traumatic brain injury (TBI) is a broad term that encompasses multiple intracranial processes (including cerebral contusion, epidural hemorrhages, subdural hemorrhages, subarachnoid hemorrhages, skull fractures, diffuse axonal injury, and cerebral edema) that occur secondary to trauma to the head or if the head experiences a sudden deceleration injury without external trauma that results in injury to the brain.1 An overview of classification of TBI is summarized in Table 1. These injuries result in varying levels of cellular and macroscopic changes, detected with clinical examination and supplemented by neuroimaging.
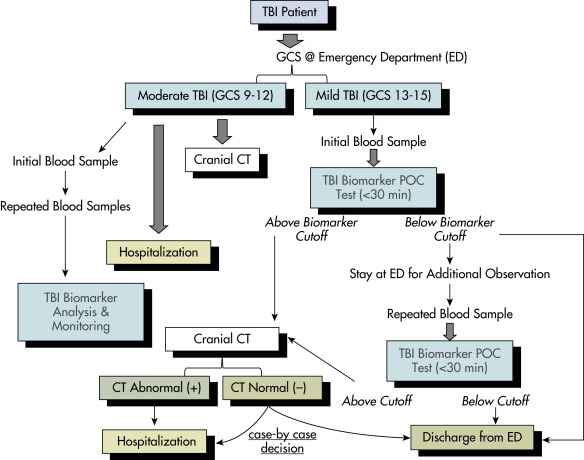
- Mild TBI is defined as loss of consciousness <30 minutes, a Glasgow Coma Scale (GCS) of 13 to 15, and normal imaging.
- Moderate TBI is defined as loss of consciousness for 30 minutes to 24 hr with even longer alteration in consciousness, a GCS of 9 to 12, and may or may not have abnormal imaging.
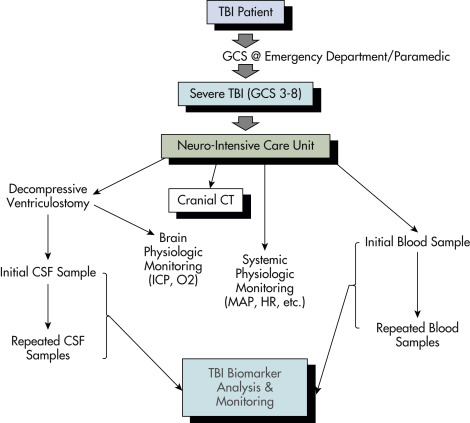
- Severe TBI is defined as >24 hr of loss of consciousness with a GCS of 3 to 8 and prolonged posttraumatic amnesia with normal or abnormal imaging.1,2
TABLE 1 Overview of Classification of Traumatic Brain Injury
Mechanism | Blunt | High velocity (MVC) Low velocity (fall, assault) | |
| Penetrating | GSW Other (stab wounds, etc.) | ||
| Blast | Explosive devices | ||
| Severity | Mild | GCS 14-15 | |
| Moderate | GCS 9-13 | ||
| Severe | GCS 3-8 | ||
| Morphology | Skull fracture | Vault | Linear versus stellate Depressed/nondepressed Open/closed |
| Basilar | With/without CSF With/without CN palsy | ||
| Intracranial lesions | Focal | Epidural Subdural Intracerebral | |
| Diffuse | Mild concussion Classic concussion Diffuse axonal injury |
CN, Cranial nerve; CSF, cerebrospinal fluid; GCS, Glasgow Coma Scale; GSW, gunshot wound; MVC, motor vehicle collision.
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
| ||||||||||||||||||||||||||||||||
Traumatic brain injury (TBI) is a worldwide leading cause of mortality in the young and elderly. In the 2017 CDC surveillance report, unintentional falls have surpassed motor vehicle crashes as number one cause of TBI.3
Globally, more than 69 million people suffer from TBI each year, with North America and Europe showing highest incidence and Southeast Asian and Western Pacific countries experiencing the greatest burden of disease. According to one estimate, up to 4.6 million individuals suffer from TBI in United States and Canada each year.4 In 2014, about 2.87 million emergency department visits, including deaths and hospitalizations, were associated with TBI. The financial burden of TBI has been estimated to be greater than $80 billion per yr in the United States alone and approaching $400 billion dollar worldwide in direct and indirect costs.5
In 2016, the global prevalence of TBI was estimated at 55.5 million. Between 1990 to 2016, the age-standardized prevalence of TBI increased by 8.4%.6 According to the CDC, there were 224,000 TBI-related hospitalization in 2017, decreased from 261,000 in 2016, while the number of deaths increased from 59,000 to 61,000.3
In the U.S. 792/100,000 individuals, including nonspecific head injury, removing which brings the number to 264/100,000.3
TBI occurs more commonly in males and hospitalizations/deaths are the highest in older adults >75 yr of age.3
TBI and Apo E Ε4 synergistically are associated with a tenfold increased risk for Alzheimer disease. Apo E Ε4 is also associated with larger intracerebral hematomas and greater ischemia after TBI.7
TBI patients can present with a spectrum of clinical symptoms including nausea, vomiting, headache, seizures, altered mental status, and/or coma. Stigmata of trauma, including bruises, scalp lacerations, and periorbital or mastoid ecchymosis suggesting skull base fractures, are telltale signs of possible underlying traumatic brain injury. Box 1 describes risk stratification in patients with minor head trauma. The spectrum of TBI is most commonly assessed using the GCS, which ranges from 3 to 15 and utilizes eye, motor, and verbal exams (Table 2).
BOX 1 Risk Stratification in Patients With Minor Head Trauma
TABLE 2 Useful Criteria to Assess the Severity of Head Injurya

| Quantifying the Degree of Head Injury | Glasgow Coma Scale (GCS) | Score |
|---|---|---|
| Eye Opening | ||
| Spontaneous | 4 | |
| To speech | 3 | |
| To pain | 2 | |
| None | 1 | |
| Verbal Response | ||
| Oriented | 5 | |
| Confused conversation | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| None | 1 | |
| Best Motor Response | ||
| Obeys commands | 6 | |
| Localizes pain | 5 | |
| Flexion withdrawal to pain | 4 | |
| Abnormal flexion (decorticate) | 3 | |
| Extension (decerebrate) | 2 | |
| None (flaccid) | 1 |
TBI, Traumatic brain injury.
a Consultation with other specialists (i.e., neurosurgeon) may be valuable for the orthopedic surgeon unfamiliar with the process of “clearing” the patient’s head injury for ischemic monomelic neuropathy (IMN) fixation.
From Browner B et al: Skeletal trauma: basic science, management, and reconstruction, ed 6, Philadelphia, 2019, Elsevier.
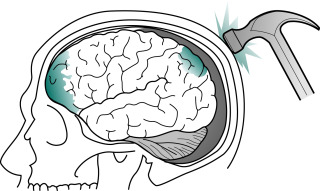
- Mechanical falls (49.1%), motor vehicle accidents (24.5%), and assaults resulting in direct or indirect trauma to the head are the most common etiologies (Fig. E1, Fig. E2).
From Kaufman DM et al: Kaufman’s clinical neurology for psychiatrists, ed 9, Philadelphia, 2023, Elsevier.
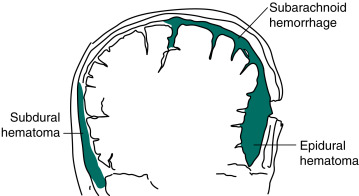
In Contrast, Venous Bleeding, Usually Slower and Under Less Pressure, Causes Subdural Hematoma. Ruptured Aneurysms and Head Trauma Often Cause Subarachnoid Hemorrhage (SAH). In SAH, Blood Spreads Within the Subarachnoid Space over the Convexities, Between the Gyri, into the Interhemispheric Fissure, and Down into the Spinal Canal.
From Kaufman DM et al: Kaufman’s clinical neurology for psychiatrists, ed 9, Philadelphia, 2023, Elsevier.
- Gunshot wounds are the most prevalent penetrating injuries (Fig. E3), accounting for 35% of deaths from TBI under the age of 45 yr in the United States. Self-inflicted injuries-for example, with nail guns-can also lead to penetrating injuries (Fig. E4). Gunshot wounds are the most lethal type of brain injury, 90% resulting in death.
Figure E3 Picture of a gunshot wound to the head-a penetrating injury.
The bullet leaves a path of destructions marked by blood, bone, and bullet fragments. Brain tissue around the bullet path is also damaged by the propagating pressure wave. However, this is not visible on computed tomography (axial computed tomography).
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia 2022, Elsevier.
This patient was neurologically intact on presentation. The difficulty in such a case is that bleeding can occur deep in the brain when the nails are removed. This patient was also at high risk for developing pseudoaneurysm later on.
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia 2022, Elsevier.
- The most common mechanisms of pediatric TBI vary according to age. Falls are the leading cause of TBI in children younger than 14 yr of age. Children younger than 4 yr of age are injured mainly by falls but are also affected by abusive injuries and motor vehicle accidents. Children 4 to 8 yr of age are injured in falls and motor vehicle accidents but also become more at risk for other transportation-related injuries such as bicycle-related incidents. Abusive head trauma (AHT) is particularly common in young infants aged less than 2 yr; approximately 30 of every 100,000 infants aged less than 1 yr were hospitalized for AHT.8
- Sports-related TBIs account for roughly one third of all causes of TBI, with males, adolescents, and young adults with higher incidence. Some common sports associated with TBI are football, horse riding, cycling, skateboarding, hockey, water sports, and snow sports.9
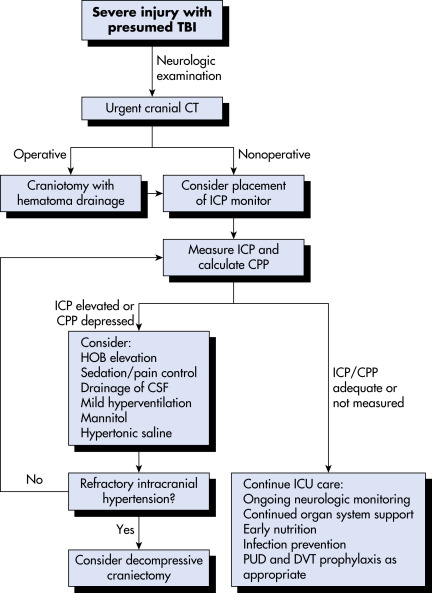
Prevention of secondary injury is the primary goal of prehospital and early in-hospital management. Most common mechanisms of secondary injury are either intracranial (increased intracranial pressure [ICP], hematoma) or systemic (hypoxia, hypovolemia, hypotension). Early categorization of head trauma patients according to the severity (based on GCS) and transport to facilities equipped with personnel and technology to deal with issues pertaining to head trauma has improved the overall management of head injury patients and prevention of secondary injury.10 Assessment and treatment recommendations for mild TBI are summarized in Table 5. Airway, breathing, and circulation, however, still remain the most important parameters to be stabilized, and both directly and indirectly affect GCS and overall outcome. Trauma guidelines suggest intubation should be performed in any patient with a GCS of 8 or less to prevent hypoxemia and hypercapnia. Previously, patients were hyperventilated to decrease pCO2 in an effort to reduce ICP. Recent evidence suggests normo-ventilation for patients with severe TBI, with hyperventilation only being used as a temporary measure until other methods of reducing ICP are employed.11 Intravenous fluid resuscitation should also be started early to prevent hypovolemia resulting in hypotension, shown to double mortality. Transfer to and care in a Level 1 trauma center are associated with better outcomes. Monitoring and treatment recommendations for severe TBI are summarized in Table 6.
TABLE 6 Guidelines for the Management of Severe Traumatic Brain Injury
| Topic | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| Blood pressure and oxygenation | Insufficient data | Avoid systolic blood pressure <90 mm Hg | Avoid hypoxia (Pao2 <60 mm Hg or O2 saturation <90%) |
| Hyperosmolar therapy | Insufficient data | Mannitol is effective for control of raised ICP at doses of 0.25 g/kg to 1 g/kg body weight | Restrict mannitol use prior to ICP monitoring in patients with signs of transtentorial herniation |
| Prophylactic hypothermia | Insufficient data | Insufficient data | Pooled data indicate that prophylactic hypothermia is not significantly associated with decreased mortality as compared with normothermic controls |
| Infection prophylaxis | Insufficient data | Periprocedural antibiotics for intubation should be administered to reduce the incidence of pneumonia Early tracheostomy should be performed to reduce days on mechanical ventilation with pneumonia | To reduce infection, routine ventricular catheter exchange or prophylactic antibiotic use for ventricular catheter placement is not recommended |
| Deep venous thrombosis prophylaxis | Insufficient data | Insufficient data | Intermittent pneumatic compression stockings are recommended Low-molecular-weight heparin or low-dose unfractionated heparin should be used in combination with mechanical prophylaxis |
| Indications for ICP monitoring | Insufficient data | ICP should be monitored in all salvageable patients with a GCS score of 3-8 after resuscitation and an abnormal CT scan | ICP monitoring is indicated in patients with severe TBI with a normal CT scan if >40 yr of age with blood pressure <90 mm Hg |
| ICP pressure-monitoring technology | N/A | N/A | N/A |
| ICP thresholds | Insufficient data | Treatment should be initiated with ICP >20 mm Hg | A combination of ICP values and clinical and brain CT findings should be used to determine the need for treatment |
| Cerebral perfusion thresholds | Insufficient data | Aggressive attempts to maintain CPP above 70 mm Hg with fluids and pressors should be avoided because of the risk of adult respiratory distress syndrome | CPP of <50 mm Hg should be avoided The CPP value to target lies within the range of 50-70 mm Hg. Patients with intact pressure autoregulation tolerate higher CPP values. Ancillary monitoring of cerebral parameters that include blood flow, oxygenation, or metabolism facilitates CPP management |
| Brain oxygen monitoring and thresholds | Insufficient data | Insufficient data | Jugular venous saturation (<50%) or brain tissue oxygen tension (<15 mm Hg) are treatment thresholds |
| Anesthetics, analgesics, sedatives | Insufficient data | Prophylactic administration of barbiturates to induce burst suppression electroencephalogram is not recommended. High-dose barbiturate administration is recommended to control elevated ICP refractory to maximum standard medical and surgical treatment. Hemodynamic stability is essential before and during barbiturate therapy. Propofol is recommended for the control of ICP but not for improvement in mortality or 6-mo outcome | N/A |
| Nutrition | Insufficient data | Patients should be fed to attain full caloric replacement by day 7 postinjury | N/A |
| Antiseizure prophylaxis | Insufficient data | Anticonvulsants are indicated to decrease the incidence of early PTS (within 7 days of injury) | N/A |
| Hyperventilation | Insufficient data | Prophylactic hyperventilation (Paco2 of 25 mm Hg or less) is not recommended | Hyperventilation is recommended as a temporizing measure for the reduction of ICP. Hyperventilation should be avoided during the first 24 hr after injury, when cerebral blood flow is often critically reduced. If hyperventilation is used, jugular venous oxygen saturation (SjO2) or brain-tissue oxygen tension (PbtO2) measurements are recommended to monitor oxygen delivery |
| Steroids | The use of high-dose methylprednisolone is associated with increased mortality and is contraindicated | N/A | N/A |
CT, Computed tomography; CPP, cerebral perfusion pressure; ICP, intracranial pressure; GCS, Glasgow Coma Scale; PTS, posttraumatic seizures; TBI, traumatic brain injury.
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.
TABLE 5 Assessment and Treatment Recommendations for Mild Traumatic Brain Injury
| Function | Assessment | Treatment |
|---|---|---|
| Overall recovery | Standardized symptom checklist | Physical rest 1-2 days1 followed by subsymptomatic aerobic exercise2 |
| Headache | Determine the type | HA persisting more than 3-4 days may require abortive treatment tailored to phenotype (migraine, tension-type, occipital neuralgia, etc.) |
| Vertigo | Romberg test, dynamic standing, tandem gait | If Hallpike Dix is normal, or if Epley maneuver does not relieve symptoms, consider physical therapy for vestibular rehabilitation |
| Eye movements | Examine cranial nerves 3, 4, 6 for tracking, saccades, diplopia, nystagmus | Physical therapy evaluation for vestibular rehabilitation |
| Near vision | Near-point accommodation and binocular convergence | Ophthalmologic evaluation for vision therapy |
| Cognitive function | Symptoms, cognitive testing, neuropsychologist evaluation | Sleep hygiene, neuropsychology evaluation for cognitive rehabilitation3 |
HA, Headache.
1 Thomas DG et al: Benefits of strict rest after acute concussion: a randomized controlled trial, Pediatrics 135:213-223, 2015.
2 Kurowski BG et al: Aerobic exercise for adolescents with prolonged symptoms after mild traumatic brain injury: an exploratory randomized clinical trial, J Head Trauma Rehabil 32:79-89, 2017.
3 Cooper DB et al: Cognitive rehabilitation for military service members with mild traumatic brain injury: a randomized clinical trial, J Head Trauma Rehabil 32:E1-E15, 2017.
From Goldman L, Schafer AI: Goldman-Cecil medicine, ed 26, Philadelphia, 2019, Elsevier.
Cpp, Cerebral Perfusion Pressure; CSF, Cerebrospinal Fluid; CT, Computed Tomography; DVT, Deep Venous Thrombosis; Hob, Head of Bed; ICP, Intracranial Pressure; ICU, Intensive Care Unit; Pud, Peptic Ulcer Disease.
From Townsend CM et al: Sabiston textbook of surgery, ed 21, St Louis, 2022, Elsevier.
Details of in-hospital management including critical care and surgical intervention is beyond the scope of this text. Some important points are summarized below.
- Advanced trauma life support (ATLS) protocol (airway, breathing, circulation, disability, exposure).
- Ventilatory support.
- Optimization of oxygenation, ventilation, and fluid status.
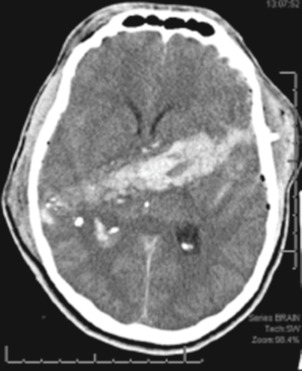
- CT head (Fig. E9) to evaluate for mass lesion (hematoma) or cerebral edema. These findings may necessitate either surgical intervention or ICP monitor placement. ATLS guidelines recommend maximum 30 minutes between initial assessment and CT head.
Figure E9 Indications for acute seizure prophylaxis in severe head trauma.
From Marx JA et al: Rosen’s emergency medicine: concepts and clinical practice, ed 7, Philadelphia, 2010, Elsevier.
- In case of either a severe TBI (GCS 8 or less) or a moderate TBI (GCS 8 to 13) with an unreliable neurologic exam, patients should be admitted to the intensive care unit for frequent neurologic checks. TBI guidelines suggest ICP monitor placement for GCS 8 or less to monitor intracranial pressure closely.11 ICP monitors are of various kinds, and the most commonly used include external ventricular drain, intraparenchymal pressure monitor, and a bolt device with brain tissue oxygen pressure monitoring with fiberoptic pressure monitor. Recent research has also supported the use of brain tissue oxygen monitoring for severe TBI patients.11
- Surgical decompression may involve evacuation of hematoma (epidural, subdural, intraparenchymal, contusion) through craniotomy alone (replacement of bone after completion of operation) versus decompressive craniectomy (complete removal of bone without replacement). Skull fractures are treated depending on the morphology of the fracture. Open, depressed fractures require surgical debridement and elevation in most cases, in addition to broad-spectrum antibiotics.
- Avoid electrolyte imbalance, especially hyponatremia and hyperglycemia, which may contribute to cerebral edema and increase intracranial pressure. A recent randomized controlled trial studied use of a continuous 20% hypertonic saline infusion vs standard therapy in patients with moderate to severe TBI (COBI trial) and did not improve neurologic status at 6 mo.12
- Elevation of head of bed to allow better venous drainage to reduce intracranial pressure.
- ICP management (Table 7), which may include the following: Drainage of cerebrospinal fluid via external ventricular drain, surgical hematoma evacuation, administration of hyperosmotic fluids to reduce edema, pharmacologic sedation and paralysis, pentobarbital-induced coma, and surgical decompression of the brain.11
- Decompressive craniectomy in patients with TBI and refractory intracranial hypertension may reduce ICU stay but does not clearly improve outcomes. DECRA13 and RESCUEicp14 are two randomized controlled trials that assessed decompressive craniectomy (DC) for reduction in ICP vs. medical management. Both trials were unable to provide definite evidence for or against DC, indicating that the decision to proceed with DC should be made on case-by-case basis, after assessment of individual risks and benefits.11
- Normothermia: In patients with TBI, hypothermia can reduce intracranial hypertension, but recent trials in patients with an intracranial pressure of more than 20 mm Hg after TBI, therapeutic hypothermia, plus standard care to reduce intracranial pressure did not result in outcomes better than those with standard care alone. The most recent TBI guidelines do not recommend hypothermia.11
- Prevention of seizures in the acute setting. Seizure prophylaxis can be considered for the first 7 days. Indications for acute seizure prophylaxis in severe head trauma are described in Box 3. Usually phenytoin or levetiracetam is used.15 Seizure prophylaxis, however, has not shown to prevent long-term development of traumatic epilepsy.
- Deep vein thrombosis (DVT) prophylaxis is recommended in almost all patients on hospital day 1 in addition to sequential compression devices (SCDs) for immobile or bedbound patients to prevent DVTs.11
- Early initiation of parenteral nutrition.
- Early tracheostomy for ventilator-dependent patients is recommended to reduce mechanical ventilation days.11
BOX 3 Indications for Acute Seizure Prophylaxis in Severe Head Trauma
TABLE 7 Elevated ICP Management
|
CBF, Cerebral blood flow; CPP, cerebral perfusion pressure; EEG, electroencephalography; EVD, external ventricular drain; ICP, intracranial pressure; MAP, mean arterial pressure; PbtO2, Brain tissue oxygen.
From Jankovic J et al: Bradley and Daroff’s neurology in clinical practice, ed 8, Philadelphia, 2022, Elsevier.