AUTHOR: Nadine N. Mbuyi, MD
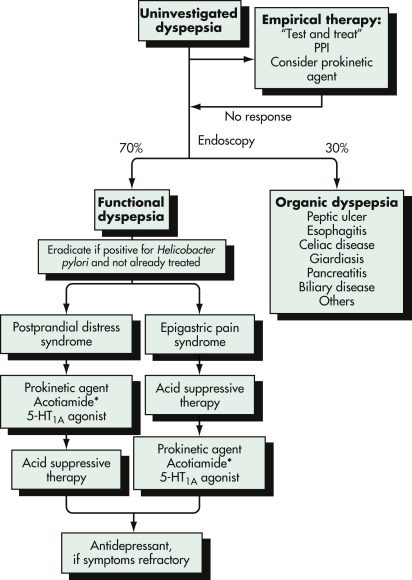
Dyspepsia is a constellation of symptoms referable to the gastroduodenal region of the upper GI tract. Nonulcerative dyspepsia is a term used to describe signs and symptoms of persistent or recurrent dyspepsia that have no identifiable organic cause.
Up to 25% of the general population will experience dyspepsia each yr. Of these, 75% will have no evident causative agent. Functional dyspepsia is a common disorder, with an estimated prevalence of 8% to 12% based on Rome IV criteria and up to 40% when less restrictive criteria are used. Data suggest that less than 15% of patients with functional dyspepsia are actually given the correct diagnosis. In the U.S., the diagnosis, treatment, and work absenteeism related to functional dyspepsia have been estimated to cost $18.4 billion per year.
Typical clinical presentation is dyspepsia without findings on physical examination to explain the symptoms.
The etiology and pathophysiology are still unclear. Box 1 summarizes causes of dyspepsia. Research is focused on abnormalities of gastric motor function and visceral hypersensitivity, as well as:
Luminal GI Tract Chronic gastric or intestinal (mesenteric) ischemia Gastric or esophageal neoplasm Gastric infections (cytomegalovirus, fungus, tuberculosis, syphilis) Gastroparesis (diabetes mellitus, postvagotomy, scleroderma, chronic intestinal pseudo-obstruction, postviral, idiopathic) Infiltrative gastric disorders (Ménétrier disease, Crohn disease, eosinophilic gastroenteritis, sarcoidosis, amyloidosis) |
From Feldman M et al (eds): Sleisenger and Fordtran’s gastrointestinal and liver disease, ed 10, Philadelphia, 2016, Elsevier.
Risk factors include the following:
- Genetic predisposition: Homozygous GNB3 gene
- Dietary habits such as caffeine, alcohol, or smoking
- Medications such as NSAIDs, calcium channel blockers, methylxanthines, alendronate, orlistat, acarbose, and potassium supplements
- Psychological disorders such as anxiety, depression, somatization, or personal history of childhood sexual or physical abuse