AUTHORS: Sarah D. Bayefsky, MD and Beth H. Rutstein, MD, MSCE
Juvenile idiopathic arthritis (JIA) is a diverse spectrum of chronic arthritides, involving arthritis of at least one joint for 6 or more wk in patients 15 yr of age or younger. Other causes of arthritis must be excluded.
Juvenile idiopathic arthritis (JIA)
| ||||||||||||||||||||||||||||||||||||||||
JIA is thought to have a global distribution. While the exact incidence and prevalence are unknown, incidence rates pooled from predominantly North American and European studies are approximately 8 per 1000 children. The predominant sex and age of patients with JIA varies by JIA subtype. The precise immunopathogenic mechanism underlying the development of disease has not been elucidated, but genetic susceptibility, environmental influences, and lifestyle modifications are all hypothesized to play a role.1
- JIA is subdivided into seven categories based on the International League of Associations for Rheumatology (ILAR) classification criteria (summarized in Table E1), all of which require the presence of chronic arthritis (arthritis for ≥6 wk). Characteristics of the various categories of JIA are summarized in Table E2
- Oligoarticular JIA (Fig. E1)
- Arthritis in ≤4 joints in the first 6 mo of disease
- Polyarticular JIA rheumatoid factor (RF)-negative polyarticular JIA
- RF-positive polyarticular JIA
- Psoriatic arthritis
- Enthesitis-related arthritis
- Undifferentiated arthritis
- Fulfills criteria in ≥2 categories above, or none of them
- Systemic JIA (sJIA)
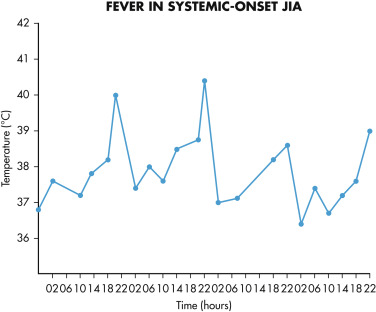
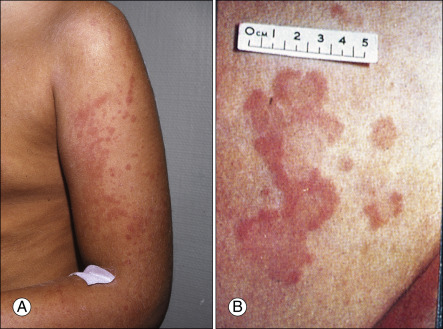
- Arthritis in ≥1 joints with, or preceded by, fever (Fig. E2) of at least 2-wk duration that is quotidian (once daily) for at least 3 days and associated with at least one of the following: (1) Evanescent rash (Fig. E3); (2) generalized lymphadenopathy; (3) hepatomegaly, splenomegaly, or both; and (4) serositis.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2018, Elsevier.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2018, Elsevier.
Figure E3 The rash of systemic juvenile idiopathic arthritis.
Larger lesions are becoming confluent (A). This must be differentiated from erythema marginatum (B), characteristic of the rash seen in rheumatic fever.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2018, Elsevier.
TABLE E1 Overview of the Main Features of the Subtypes of Juvenile Idiopathic Arthritis
| ILAR Subtype | Peak Age of Onset (yr) | Female:Male | Arthritis Pattern | Extraarticular Features | Investigations | Therapy |
|---|---|---|---|---|---|---|
| Oligoarticular | 1-3 | 4:1 | Knees >ankles | Uveitis in ∼20% | ANA positive in 60%; inflammatory markers are usually normal or only slightly ↑ | NSAIDs and intraarticular steroids; MTX |
| Polyarticular, RF negative | 1-3 and 9-14 (biphasic) | 3:1 | Symmetric or asymmetric; small and large joints; cervical spine; TMJ | Uveitis in ∼10% | ANA positive in 40%; RF negative; may have elevated inflammatory markers and anemia of chronic disease | MTX and NSAIDs as first-line; often require TNF inhibitors or other biologics |
| Polyarticular, RF positive | 9-11 | 9:1 | Aggressive symmetric polyarthritis, especially of the small joints (wrists, hands) | Rheumatoid nodules in 10% | RF positive; CCP positive (60%); elevated inflammatory markers and anemia of chronic disease | MTX, TNF inhibitors, other biologics. Long-term remission off medication is unlikely; early aggressive therapy is warranted |
| Psoriatic | 2-3 and mid-adolescence (biphasic) | 2:1 in younger patients; 1:1 in older children | Asymmetric arthritis (oligoarthritis >polyarthritis) of small and medium-sized joints; sacroiliitis in 10%-30% | Psoriasis in 40%-66%; uveitis in 10%-15%; dactylitis and enthesitis common; comorbid obesity | ANA positive in 50%; inflammatory markers normal or mildly elevated | MTX, TNF inhibitors, and other biologics; NSAIDs and intraarticular steroids as needed can consider anti-IL-17 or anti-IL-12/23 therapy |
| Enthesitis-related arthritis | 10-13 | 1:4 | Predominantly asymmetric, lower limb arthritis; sometimes axial skeleton (but less than adult AS) | Enthesitis in 60%-80%; acute anterior uveitis; association with IBD | 60%-90% HLA-B27 positive | NSAIDs and intraarticular steroids; consider sulfasalazine, MTX; TNF inhibitors if needed |
| Systemic | 2-4 | 1:1 | Polyarticular, often knees, wrists, and ankles; also fingers, neck, and hips | Daily fever; evanescent rash; pericarditis; pleuritis; hepatomegaly; splenomegaly; lymphadenopathy | Anemia; ↑WBC; ↑ESR; ↑CRP; ↑ferritin; ↑platelets (normal or ↓in MAS) | Standing NSAIDs; IL-1 antagonists; systemic steroids |
ANA, Antinuclear antibody; AS, ankylosing spondylitis; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; IBD, inflammatory bowel disease; ILAR, International League of Associations for Rheumatology; IL-1, interleukin-1 ; JIA, juvenile idiopathic arthritis; MAS, macrophage activation syndrome; MTX, methotrexate; NSAID, nonsteroidal antiinflammatory drug; RF, rheumatoid factor; TMJ, temporomandibular joint; TNF, tumor necrosis factor; WBC, white blood cell count.
TABLE E2 Characteristics of the Various Categories of Juvenile Idiopathic Arthritis
| Category | Age at Onset | Affected Joints | Systemic Features | Major Complications |
|---|---|---|---|---|
| Oligoarticular persistent | Early childhood | Large joints, asymmetric (knee, ankle, wrist, elbow, temporomandibular, cervical spine) | No | Chronic uveitis Local growth disturbances |
| Oligoarticular extended | Early childhood | Same as above, but more than four joints involved after the first 6 mo of disease | No | Chronic uveitis Local growth disturbances |
| Polyarticular RF negative | Throughout childhood | Any, often symmetric, often small joints | Malaise (subfebrile) | Chronic uveitis Local growth disturbances |
| Polyarticular RF positive | Teenage years | Any, usually symmetric and involving small joints | Malaise (subfebrile) | Local growth disturbances and articular damage |
| Psoriatic | Late childhood | Spine, lower extremities, distal interphalangeal joints, dactylitis | Psoriasis | Psoriasis Local growth disturbances |
| Enthesitis-related | Late childhood | Spine, sacroiliac, lower extremities, thoracic cage joints | Inflammatory bowel disease | Acute symptomatic uveitis |
| Systemic | Throughout childhood | Any (not necessarily at disease onset) | High fever, rash, polyserositis, hepatosplenomegaly; lymphadenopathy; marked acute-phase response | Acute: Macrophage activation syndrome Chronic: General growth disturbance, amyloidosis |
RF, Rheumatoid factor.
From Hochberg MC: Rheumatology, ed 7, Philadelphia, 2018, Elsevier.