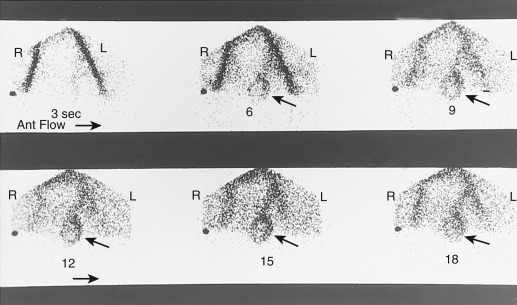
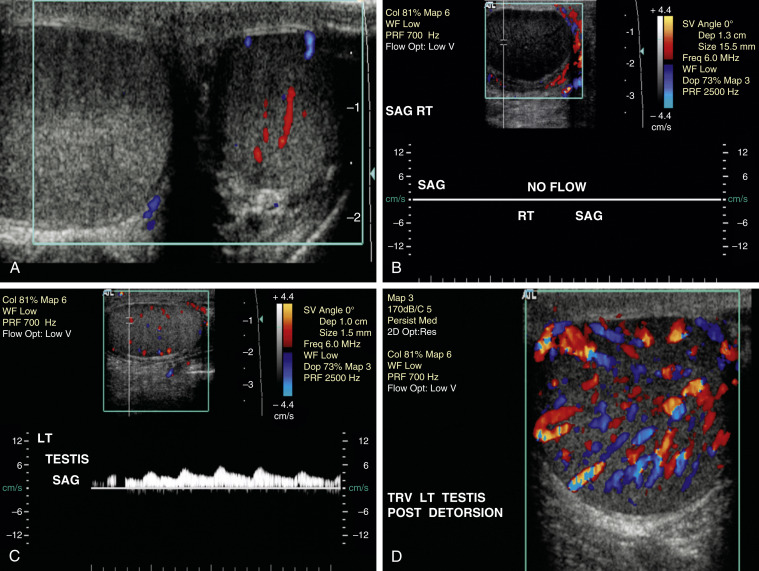
Diagnosis made mainly by clinical suspicion (Table E1). Color Doppler ultrasound evaluation or a nuclear testicular scan (Figs. E2 and E3) may help with diagnosis. Ultrasonography shows absent or decreased blood flow; scintigraphy reveals decreased perfusion on symptomatic side.
TABLE E1 Differentiation of Testicular Torsion, Epididymitis, and Appendage Torsion
| Testicular Torsion | Epididymitis∗ | Appendage Torsion |
|---|
| Historical Features |
| Age | Peak incidence in neonatal and adolescent groups but may occur at any age | Primarily adolescents and adults but may occur at any age | Typically prepubertal boys |
| Risk factors | Undescended testicle (neonate), rapid increase in testicular size (adolescent), failure of previous orchiopexy | Sexual activity or promiscuity, GU anomalies, GU instrumentation | Presence of appendages |
| Pain onset | Sudden | Gradual | Gradual or sudden |
| Previous episodes of similar pain | Possible (spontaneous detorsion) | Unlikely | Occasional |
| History of trauma | Possible | Possible | Possible |
| Nausea, vomiting | More likely | Less likely | Less likely |
| Dysuria | Less likely | More likely | Less likely |
| Physical Findings |
| Fever | Less likely | More likely, particularly with advanced disease (epididymo-orchitis) | Less likely |
| Location of swelling and tenderness | Testicle, progressing to diffuse hemiscrotal involvement | Epididymis, progressing to diffuse hemiscrotal involvement | Localized to head of affected testicle or epididymis |
| Cremasteric reflex | Testicular torsion less likely if present | May be present or absent | May be present or absent |
| Testicle position | High-riding testicle, transverse alignment | Normal position, vertical alignment | Normal position, vertical alignment |
| Pyuria | Less likely | More likely | Less likely |
GU, Genitourinary.
From Adams JG et al: Emergency medicine, clinical essentials, ed 2, Philadelphia, 2013, Elsevier.
Figure E2 Testicular torsion.
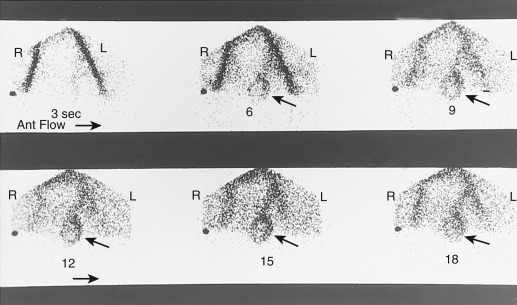
Evaluation of blood flow to the testicle has been done by giving an intravenous bolus of radioactive material. The right and left iliac vessels are clearly identified, and sequential images are obtained every 3 seconds. Here, increased flow is seen to the rim of the left testicle (arrows), and there is no blood flow centrally. This is the appearance of a testicular torsion in which the torsion has been present for more than approximately 24 hr. Ant, Anterior.
From Mettler FA [ed]: Primary care radiology, Philadelphia, 2000, Saunders.
Figure E3 Acute testicular torsion.
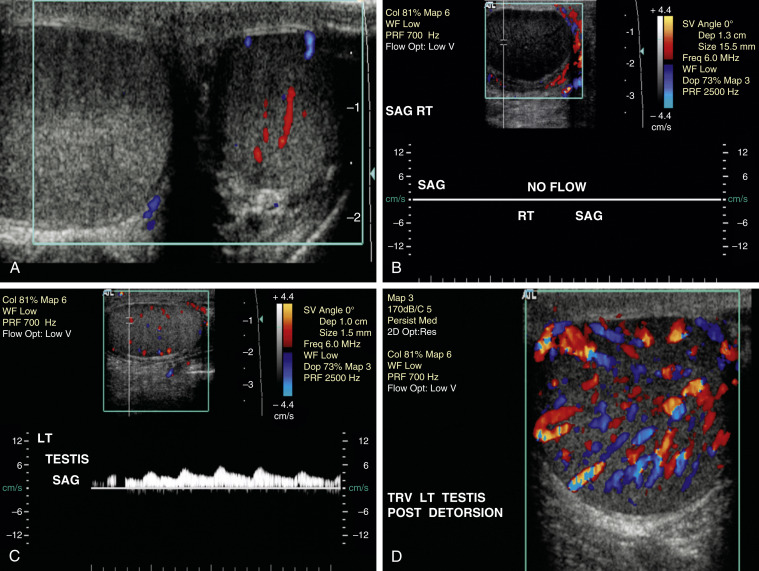
A to C, This 13-yr-old boy presented with acute, excruciating right-sided scrotal pain. A, Transverse gray-scale image of both testes demonstrates enlargement of the avascular right testis. B, Absence of both color and pulsed Doppler flow is noted on this sagittal image of the right testis. C, Normal pulsed and color Doppler flow confirmed in asymptomatic, normal-appearing left testis. D, Teenage boy with acute left-sided testicular torsion. Closed manual detorsion of the left testis was done at diagnosis in the ultrasound suite. Color Doppler sonogram of the left testis obtained immediately after detorsion shows dramatic hyperemia throughout the left testis. LT, Left; RT, right; SAG, sagittal; TRV, transverse.
From Rumack CM et al: Diagnostic ultrasound, ed 4, Philadelphia, 2011, Elsevier.
Differential Diagnosis
- Torsion of the testicular appendages (appendix testis)
- Testicular tumor
- Epididymitis
- Incarcerated inguinoscrotal hernia
- Orchitis
- Spermatocele
- Hydrocele, varicocele
WorkupThe diagnosis is usually based on history and physical examination.
Imaging Studies
- Doppler ultrasonic stethoscope (Doppler flowmetry) (Fig. E3)
- Radionuclide scrotal scanning (technetium-99m): Cold testicle (Fig. E2)