Chronic Primary MR:
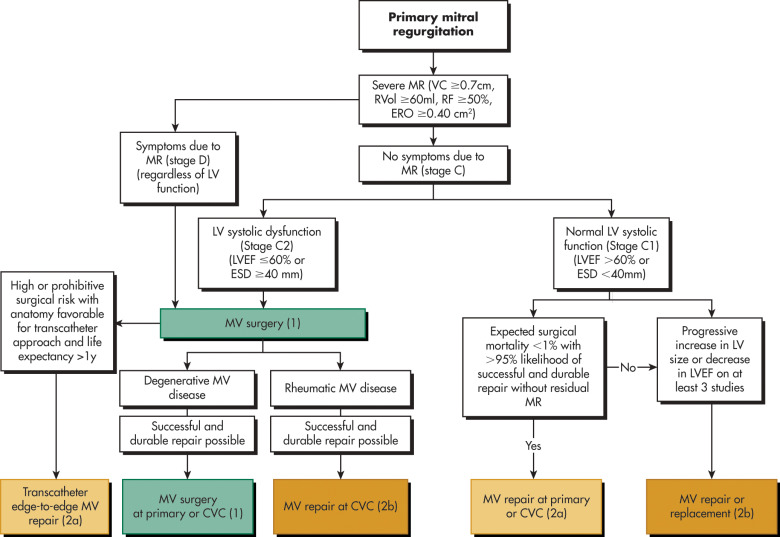
- Medical Therapy: While useful in acute severe MR, there is no evidence of vasodilator reducing severity in chronic primary MR. Guideline-directed medical therapy (GDMT) can be helpful in patients who are unable to undergo surgery to treat LV dysfunction. Stages of chronic primary mitral regurgitation are outlined in Table E1. Fig. 3 and Table E2 illustrate management strategy for intervention for primary MR.
- Surgical Intervention: Surgery is the only definitive treatment for MR. Although no randomized trial of mitral valve repair vs. replacement exists, repair is favored over replacement4 in degenerative mitral valve disease due to its lower perioperative risk, improved event-free survival, freedom from complications of prosthetic valves, and better postoperative LV function.
- Surgery is a class I recommendation in patients with the following diagnoses:
- Symptomatic patients with severe primary MR irrespective of LV systolic function.
- Asymptomatic patients with severe primary MR and LV systolic dysfunction (left ventricular ejection fraction [LVEF] ≤60%) or progressive dilation (left ventricular end-systolic diameter [LVESD] ≥40 mm).
- Surgery is a class IIa recommendation in:
- Asymptomatic severe MR with normal LV systolic function (LVEF ≥60% and LVESD ≤40 mm) in whom the likelihood of successful repair without residual MR is >95% and operative mortality is <1%.
- Severely symptomatic patients (New York Heart Association [NYHA] class III/IV) with primary severe MR and high surgical risk, transcatheter edge to edge repair is reasonable if patient life expectancy is at least 1 yr.
- Surgery is a class IIb recommendation in:
- Asymptomatic patients with severe primary MR and normal LV systolic function but with progressive increase in LV size or decrease in ejection fraction (EF) on three or more serial imaging studies.
- Symptomatic patients with severe primary MR due to rheumatic valve disease, mitral valve repair may be considered if surgical treatment is indicated and successful repair is likely.
Figure 3 Management strategy for intervention for primary mitral regurgitation.

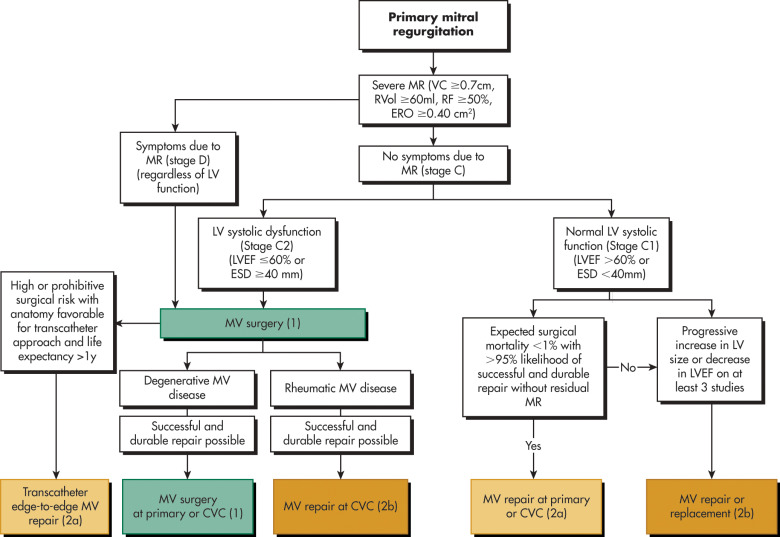
Colors correspond to Table E2. CVC, Comprehensive valve center; ERO, effective regurgitant orifice; ESD, end-systolic dimension; LVEF, ejection fraction; MR, mitral regurgitation; MV, mitral valve; MVR, mitral valve replacement; RF, regurgitant fraction; RVol, regurgitant volume; VC, vena contracta.
(From Otto CM et al: 2020 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, J Am Coll Cardiol 77:e25-e197, 2021. In Libby P et al: Braunwald’s heart disease, a textbook of cardiovascular medicine, ed 12, Philadelphia, 2022, Elsevier.)
TABLE E1 Stages of Chronic Primary Mitral Regurgitation
| Stage | Definition | Valve Anatomy | Valve Hemodynamics* | Hemodynamic Consequences | Symptoms |
|---|
| A | At risk for MR | - Mild MVP with normal coaptation
- Mild valve thickening and leaflet restriction
| - No MR jet or small central jet area <20% LA on Doppler
- Small vena contracta <0.3 cm
| None | None |
| B | Progressive MR | - Moderate to severe MVP with normal coaptation
- Rheumatic valve changes with leaflet restriction and loss of central coaptation
- Previous IE
| - Central jet MR 20%-40% LA or late systolic eccentric jet MR
- Vena contracta <0.7 cm
- Rvol <60 ml
- RF <50%
- ERO <0.40 cm 2
- Angiographic grade 1-2+
| - Mild LA enlargement
- No LV enlargement
- Normal pulmonary pressure
| None |
| C | Asymptomatic severe MR | - Severe MVP with loss of coaptation or flail leaflet
- Rheumatic valve changes with leaflet restriction and loss of central coaptation
- Previous IE
- Thickening of leaflets with radiation heart disease
| - Central jet MR >40% LA or holosystolic eccentric jet MR
- Vena contracta ≥0.7 cm
- Rvol ≥60 ml
- RF ≥50%
- ERO ≥0.40 cm 2
- Angiographic grade 3-4+
| - Moderate or severe LA enlargement
- LV enlargement
- Pulmonary hypertension may be present at rest or with exercise.
- C1: LVEF >60% and LVESD <40 mm
- C2: LVEF ≤60% and LVESD ≥40 mm
| None |
| D | Symptomatic severe MR | - Severe MVP with loss of coaptation or flail leaflet
- Rheumatic valve changes with leaflet restriction and loss of central coaptation
- Previous IE
- Thickening of leaflets with radiation heart disease
| - Central jet MR >40% LA or holosystolic eccentric jet MR
- Vena contracta ≥0.7 cm
- Rvol ≥60 ml
- RF ≥50%
- ERO ≥0.40 cm 2
- Angiographic grade 3-4+
| - Moderate or severe LA enlargement
- LV enlargement
- Pulmonary hypertension present
| - Decreased exercise tolerance
- Exertional dyspnea
|
ERO, Effective regurgitant orifice; IE, infective endocarditis; LA, left atrium; LV, left ventricle; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic dimension; MR, mitral regurgitation; MVP, mitral valve prolapse; RF, regurgitant fraction; Rvol, regurgitant volume.
From Otto CM et al: 2020 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, J Am Coll Cardiol 77:e25-197, 2021. In Libby P et al: Braunwald’s heart disease, a textbook of cardiovascular medicine, ed 12, Philadelphia, 2022, Elsevier.
TABLE E2 Recommendations for Intervention for Chronic Primary Mitral Regurgitation
| Cor | Loe | Recommendations |
|---|
| 1 | B-NR | - In symptomatic patients with severe primary MR (stage D), mitral valve intervention is recommended irrespective of LV systolic function.
|
| 1 | B-NR | - In asymptomatic patients with severe primary MR and LV systolic dysfunction (LVEF ≤60%, LVESD ≥40 mm) (stage C2), mitral valve surgery is recommended.
|
| 1 | B-NR | - In patients with severe primary MR for whom surgery is indicated, mitral valve repair is recommended in preference to mitral valve replacement when the anatomic cause of MR is degenerative disease, if a successful and durable repair is possible.
|
| 2a | B-NR | - In asymptomatic patients with severe primary MR and normal LV systolic function (LVEF ≥60% and LVESD ≤40 mm) (stage C1), mitral valve repair is reasonable when the likelihood of a successful and durable repair without residual MR is >95% with an expected mortality rate of <1%, when it can be performed at a primary or comprehensive valve center.
|
| 2b | C-LD | - In asymptomatic patients with severe primary MR and normal LV systolic function (LVEF >60% and LVESD <40 mm) (stage C1) but with a progressive increase in LV size or decrease in EF on ≥3 serial imaging studies, mitral valve surgery may be considered irrespective of the probability of a successful and durable repair.
|
| 2a | B-NR | - In severely symptomatic patients (NYHA Class III or IV) with primary severe MR and high or prohibitive surgical risk, transcatheter edge-to-edge repair (TEER) is reasonable if mitral valve anatomy is favorable for the repair procedure and patient life expectancy is at least 1 yr.
|
| 2b | B-NR | - In symptomatic patients with severe primary MR attributable to rheumatic valve disease, mitral valve repair may be considered at a comprehensive valve center by an experienced team when surgical treatment is indicated, if a durable and successful repair is likely.
|
| 3: Harm | B-NR | - In patients with severe primary MR in which leaflet pathology is limited to less than half the posterior leaflet, mitral valve replacement should not be performed unless mitral valve repair has been attempted at a primary or comprehensive valve center and was unsuccessful.
|
EF, Ejection fraction; LV, left ventricle; LVEF, LV ejection fraction; LVESD, LV end-systolic dimension; MR, mitral regurgitation; NYHA, New York Heart Association.
From Otto CM et al: 2020 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, J Am Coll Cardiol 77:e25-197, 2021. In Libby P et al: Braunwald’s heart disease, a textbook of cardiovascular medicine, ed 12, Philadelphia, 2022, Elsevier.
Chronic Secondary MR:
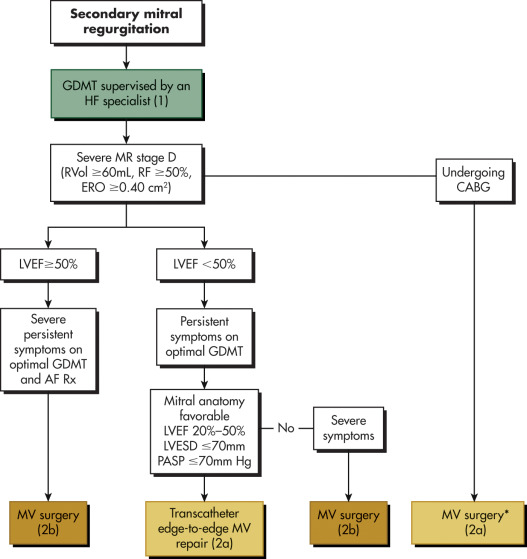
- Medical Therapy: Because secondary MR usually develops due to LV systolic dysfunction, GDMT is mainstay of therapy. It is often responsive to GDMT and reduces the severity of secondary MR. Coronary revascularization or cardiac revascularization can be considered. Stages of chronic secondary mitral regurgitation are outlined in Table E3. Table E4 and Fig. E4 illustrate management strategy for intervention for secondary MR.
- Surgical Intervention: In chronic secondary MR, appropriate and proper trial with GDMT is crucial before determining necessity for surgical or transcatheter interventions.
- Surgery is a class IIa recommendation in:
- Chronic severe secondary MR related to LV systolic dysfunction of EF <50% with persistent symptoms (NYHA class II/III/IV) while on optimal GDMT for HF. If mitral anatomy is favorable on TEE, transcatheter edge-to-edge repair (TEER) is reasonable.
- Severe secondary MR when coronary artery bypass graft (CABG) was undertaken for myocardial ischemia.
- Surgery is a class IIb (reasonable) recommendation in:
- Chronic severe secondary MR from atrial annular dilation with EF ≥50% with severe persistent symptoms (NYHA class III/IV) despite therapy for heart failure (HF), atrial fibrillation (AF), or other comorbidities.
- Chronic severe secondary MR with LEVF<50% and persistent severe symptoms (NYHA class III/IV) on optimal GDMT. In these patients with CAD, chordal sparing MV replacement may be reasonable over downsized annuloplasty repair.
Figure E4 Management strategy for intervention for secondary mitral regurgitation.

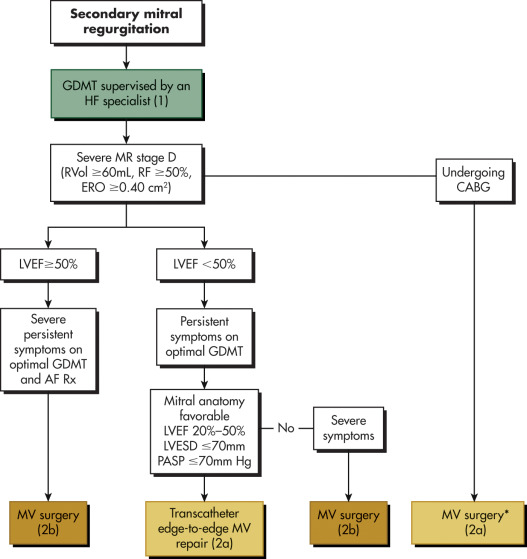
Colors correspond to Table E4. AF, Atrial fibrillation; CABG, coronary artery bypass graft; ERO, effective regurgitant orifice; GDMT, guideline-directed management and therapy; HF, heart failure; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic dimension; MR, mitral regurgitation; MV, mitral valve; PASP, pulmonary artery systolic pressure; RF, regurgitant fraction; Rvol, regurgitant volume; Rx, medication.
(From Otto CM et al: 2020 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, J Am Coll Cardiol 77:e25-197, 2021. In Libby P et al: Braunwald’s heart disease, a textbook of cardiovascular medicine, ed 12, Philadelphia, 2022, Elsevier.)
TABLE E3 Stages of Chronic Secondary Mitral Regurgitation
| Stage | Definition | Valve Anatomy | Valve Hemodynamics* | Associated Clinical Findings | Symptoms |
|---|
| A | At risk of MR | - Normal valve leaflets, chords, and annulus in a patient with coronary disease or cardiomyopathy
| - No MR jet or small central jet area <20% LA on Doppler
- Small vena contracta <0.30 cm
| - Normal or mildly dilated LV size with fixed (infarction) or inducible (ischemia) regional wall motion abnormalities
- Primary myocardial disease with LV dilation and systolic dysfunction
| Symptoms attributable to coronary ischemia or HF may be present that respond to revascularization and appropriate medical therapy |
| B | Progressive MR | - Regional wall motion abnormalities with mild tethering of mitral leaflet
- Annular dilation with mild loss of central coaptation of the mitral leaflets
| - ERO †<0.40 cm 2
- Rvol <60 ml
- RF <50%
| - Regional wall motion abnormalities with reduced LV systolic function
- LV dilation and systolic dysfunction attributable to primary myocardial disease
| Symptoms attributable to coronary ischemia or HF may be present that respond to revascularization and appropriate medical therapy |
| C | Asymptomatic severe MR | - Regional wall motion abnormalities and/or LV dilation with severe tethering of mitral leaflet
- Annular dilation with severe loss of central coaptation of the mitral leaflets
| - ERO †≥0.40 cm 2
- Rvol ≥60 ml
- RF ≥50%
| - Regional wall motion abnormalities with reduced LV systolic function
- LV dilation and systolic dysfunction attributable to primary myocardial disease
| Symptoms attributable to coronary ischemia or HF may be present that respond to revascularization and appropriate medical therapy |
| D | Symptomatic severe MR | - Regional wall motion abnormalities and/or LV dilation with severe tethering of mitral leaflet
- Annular dilation with severe loss of central coaptation of mitral leaflets
| - ERO †≥0.40 cm 2
- Rvol ≥60 ml
- RF ≥50%
| - Regional wall motion abnormalities with reduced LV systolic function
- LV dilation and systolic dysfunction attributable to primary myocardial disease
| - HF symptoms attributable to MR persist even after revascularization and optimization of medical therapy
- Decreased exercise tolerance
- Exertional dyspnea
|
ERO, Effective regurgitant orifice; HF, heart failure; LA, left atrium; LV, left ventricular; MR, mitral regurgitation; RF, regurgitant fraction; Rvol, regurgitant volume.
From Otto CM et al: 2020 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, J Am Coll Cardiol 77:e25-197, 2021. In Libby P et al: Braunwald’s heart disease, a textbook of cardiovascular medicine, ed 12, Philadelphia, 2022, Elsevier.
TABLE E4 Recommendations for Intervention for Chronic Secondary Mitral Regurgitation
| Cor | Loe | Recommendations |
| 2a | B-R | - In patients with chronic severe secondary MR related to LV systolic dysfunction (LVEF <50%) who have persistent symptoms (NYHA Class II, III, or IV) while on optimal GDMT for HF (stage D), TEER is reasonable in patients with appropriate anatomy as defined on TEE and with LVEF between 20% and 50%, LVESD ≤70 mm, and pulmonary artery systolic pressure ≤70 mm Hg.
|
| B-NR | - In patients with severe secondary MR (stages C and D), mitral valve surgery is reasonable when CABG is undertaken for the treatment of myocardial ischemia.
|
| 2b | B-NR | - In patients with chronic severe secondary MR from atrial annular dilation with preserved LV systolic function (LVEF ≥50%) who have severe persistent symptoms (NYHA Class III or IV) despite therapy for HF and therapy for associated AF or other comorbidities (stage D), mitral valve surgery may be considered.
|
| B-NR | - In patients with chronic severe secondary MR related to LV systolic dysfunction (LVEF <50%) who have persistent severe symptoms (NYHA class III or IV) while on optimal GDMT for HF (stage D), mitral valve surgery may be considered.
|
| B-R | - In patients with CAD and chronic severe secondary MR related to LV systolic dysfunction (LVEF <50%) (stage D) who are undergoing mitral valve surgery because of severe symptoms (NYHA class III or IV) that persist despite GDMT for HF, chordal-sparing mitral valve replacement may be reasonable to choose over downsized annuloplasty repair.
|
CABG, Coronary artery bypass graft; CAD, coronary artery disease; GDMT, guideline-directed medical therapy; HF, heart failure; LVEF, left ventricular ejection fraction; LVESD, left ventricular end-systolic dimension; MR, mitral regurgitation; NYHA, New York Heart Association; TEE, transesophageal echocardiography; TEER, transcatheter edge-to-edge repair.