Author: Glenn G. Fort, MD, MPH
Arthropod-borne viruses (arboviruses) are transmitted to humans primarily through the bites of infected mosquitoes. West Nile virus (WNV) is the leading cause of domestically acquired arboviral disease in the U.S.
- WNV
- West Nile virus fever
- West Nile virus encephalitis
- Neuroinvasive West Nile virus infection
- Nonneuroinvasive West Nile virus infection
| ||||||||
- Before 1999, WNV infection was confined to areas in the Middle East, with occasional outbreaks in Europe. The infection began being diagnosed in the Western Hemisphere in 1999. First seen in the northeast and mid-Atlantic states, WNV virus infection has spread steadily each year to new regions of the U.S., with a general westward migration pattern. Since 2004, the incidence of WNV infection waxed and waned as it spread to the western states. Human cases of WNV infection have now been reported across all the contiguous continental U.S. (sparing only Hawaii and Alaska).
- From 1999 through 2016, more than 780,000 cases of WNV infection occurred in the U.S., with 21,574 cases of neuroinvasive disease and 2017 deaths attributable to WNV. The overall mortality rate from reported cases of symptomatic patients with WNV is ~4%. The virus has now become the most prevalent, reportable, arthropod-borne form of viral encephalitis in North America and is likely to remain for decades to come. In 2019, 47 states and the District of Columbia reported 958 cases of WNV, of which 626 cases were neuroinvasive WNV disease (e.g., meningitis, encephalitis, acute flaccid paralysis) and 332 cases were noninvasive disease, for a national incidence of 0.44 cases/100,000 population. California, Arizona, and Colorado had the highest reported numbers of cases. In 2021 there 2911 cases of West Nile infection and in 2022 the number of cases was 1126 in the US.
- The virus is carried by a number of species of birds, as well as horses and several other animals. It is transmitted to humans through the bite of an infected mosquito. For this reason, WNV infection is seen primarily from mid-summer to mid-autumn, the period of maximum mosquito intensity (Fig. E1).
- The majority of severe cases have been reported among individuals >50 yr of age. There is no sex predilection. Certain human leukocyte antigen (HLA) haplotypes appear to predispose to severe disease (e.g., HLA-A68 and HLA-C08).
- Person-to-person transmission is fortunately rare but has been reported to occur by blood transfusion, organ transplantation, breastfeeding, and perhaps perinatal transmission; the blood supply is now routinely tested by nucleic acid testing methods to reduce the risk of transmission-acquired WNV in the U.S.
Figure E1 West Nile Virus Transmission Cycle as an Exemplar of Mosquito-Avian-Virus Transmission Cycle and the Ecologic, Virologic, Vector, and Human Factors Impacting Exposure, Infection, and Infection Outcomes
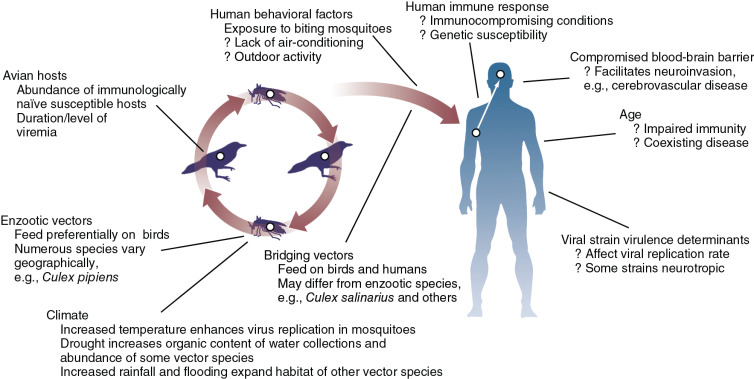
(From Bennett JE et al: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, ed 9, Philadelphia, 2020, Elsevier.)
- Less than 20% of infected individuals develop symptomatic disease, and less than 1% of infected persons develop neuroinvasive disease. The initial phase of illness is nonspecific, with abrupt onset of fever (West Nile fever) accompanied by malaise, eye pain, anorexia, headache, and, occasionally, rash and lymphadenopathy. Less commonly, myocarditis, hepatitis, or pancreatitis may occur.1
- Encephalitis is the most common neurologic manifestation of WNV infection. Aseptic meningitis may also occur.
- In ~1/150 cases, especially among older patients (>70 yr), severe neurologic sequelae will occur (West Nile neuroinvasive disease [WNND]). Most common among these are ataxia, cranial nerve palsies, optic neuritis, seizures, myelitis, and polyradiculitis.
The WNV is a member of the flavivirus group, along with the yellow fever, dengue, St Louis, and Japanese encephalitis viruses. It has a large reservoir in nature, infecting many species of birds, as well as certain mammals, and is spread to humans primarily by the bite of an infected Culex mosquito or other various species of mosquito, with a peak incidence in the late summer and early fall. Neurologic disease is caused by direct invasion of the CNS.